
Navigating AHCCCS Changes: What Behavioral Health Practices Need to Know
October 30, 2024In October 2024, the Arizona Health Care Cost Containment System (AHCCCS) introduced key updates that directly impact behavioral health practices. These changes, centered around service delivery and billing procedures, are designed to improve care efficiency and reimbursement while promoting integrated care models.
At John Lynch & Associates, our team of experienced consultants is uniquely equipped to help your practice adapt to these changes seamlessly. With deep expertise in Revenue Cycle Management (RCM), EHR consulting, and healthcare regulatory compliance, we can assist your practice in understanding and implementing the latest AHCCCS requirements, ensuring that you remain compliant and efficient while providing excellent care.
Here’s a breakdown of how these updates affect behavioral health practices and tips for adapting to provide excellent care moving forward.
Key Changes Impacting Behavioral Health Practices
1. Rate Adjustments
While behavioral health-specific fee schedules remain unchanged, several other updates may indirectly affect practices that offer integrated care. Federally Qualified Health Centers (FQHCs), hospice care, and other primary care services saw rate adjustments that could influence behavioral health practices working in collaboration with these services. Keeping up to date with rate schedules is essential for ensuring proper billing and compliance.
Resources:
Final Notice of Public Information
2. Telehealth Expansion
AHCCCS expanded telehealth offerings for Intensive Outpatient Programs (IOP), a change that allows practices to provide more flexible and accessible care. This is especially relevant for rural areas or patients who may face barriers to in-person care. By incorporating telehealth, practices can offer continuous care while complying with AHCCCS guidelines on remote services.
Resources:
Final Notice of Public Information
AZ Behavioral Health Association
3. Peer Support and Case Management Changes
One of the more significant changes for behavioral health providers is the closure of the per diem billing code for peer support, moving instead to a 15-minute billing increment. Additionally, the introduction of Behavioral Health Outreach Services within case management expands the scope of care coordination that behavioral health providers can offer. This update emphasizes the importance of robust documentation and enhanced service tracking.
Resources:
Final Notice of Public Information
AZ Behavioral Health Association
4. New Doula Services Fee Schedule
A new fee schedule was introduced for doula services, reflecting a growing recognition of the need for comprehensive perinatal care, which often intersects with behavioral health services for pregnant women and new mothers. This allows behavioral health practices that offer maternal mental health support to incorporate doula services as part of an integrated care approach.
Resources:
Final Notice of Public Information
Tips for Behavioral Health Practices Moving Forward
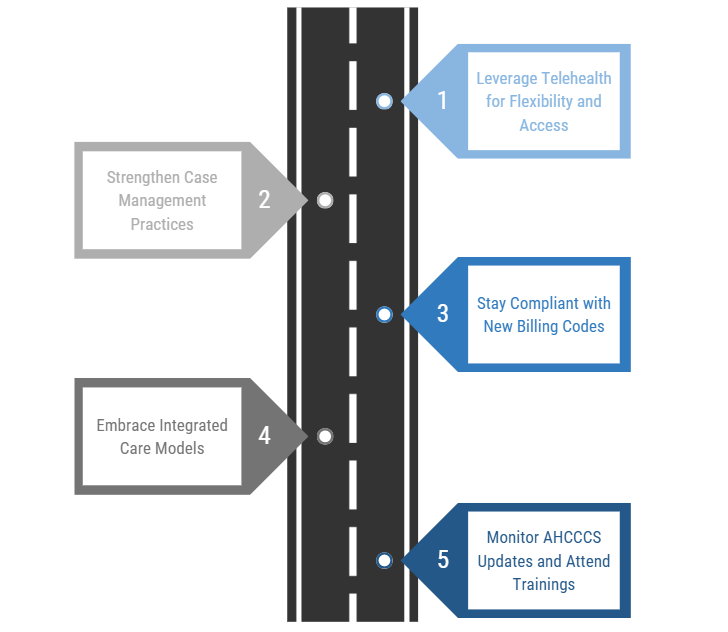
1. Leverage Telehealth for Flexibility and Access
With the expansion of telehealth, practices should integrate virtual care into their service models. By using telehealth for IOP and other services, practices can reduce no-show rates, enhance continuity of care, and reach patients in rural or underserved areas. Make sure to invest in HIPAA-compliant telehealth platforms and train both staff and patients on their use.
Resources:
AHCCCS Tackling Housing Instability with Their New ‘H2O’ Program
2. Strengthen Case Management Practices
The updated guidelines around Behavioral Health Outreach Services within case management highlight the growing importance of coordinated care. Practices should streamline workflows to ensure efficient communication between teams and document services effectively to meet AHCCCS requirements. This will not only improve patient outcomes but also enhance billing accuracy and reimbursement rates.
Resource:
AZ Behavioral Health Association
3. Stay Compliant with New Billing Codes
With the transition from per diem codes to 15-minute increments for peer support, practices must update their billing systems and staff training. Accurate billing ensures that services are reimbursed at the correct rates and helps avoid claim denials. Regular staff training on these changes can reduce errors and improve overall compliance.
Resource:
Final Notice of Public Information
4. Embrace Integrated Care Models
AHCCCS is increasingly promoting integrated care models, combining behavioral health and physical health services. Behavioral health practices should explore partnerships with primary care providers or offer integrated services in-house. This approach aligns with value-based payment models, which link reimbursement to patient outcomes rather than service volume.
Resources:
AHCCCS Tackling Housing Instability with Their New ‘H2O’ Program
5. Monitor AHCCCS Updates and Attend Trainings
AHCCCS frequently holds public meetings and training sessions to help providers stay informed on policy updates. Participating in these sessions ensures that practices remain compliant and can take advantage of new opportunities. For example, AHCCCS is offering specific training in the updated Covered Behavioral Health Services Guide.
Resource:
AZ Behavioral Health Association
Conclusion
The October 2024 AHCCCS updates present both challenges and opportunities for behavioral health practices. John Lynch & Associates can guide your practice through the new AHCCCS landscape by offering tailored consulting services.
By staying informed and adapting to these changes, practices can ensure compliance, improve patient care, and optimize reimbursement. Prioritizing telehealth, enhancing case management, and embracing integrated care models will position behavioral health providers for success in the evolving healthcare landscape.
Whether you need help with adjusting your billing processes, integrating telehealth more effectively, or enhancing your case management systems, our consultants provide the expertise and support needed to ensure success.
We partner with behavioral health practices to navigate regulatory shifts while optimizing operations, positioning you to deliver superior patient care. With John Lynch & Associates by your side, you can confidently navigate the evolving AHCCCS guidelines and thrive in today’s healthcare environment. Contact us here or speak with an expert at 623.980.8018.
