
Interoperability: Solving Staffing & Operations in Ambulatory Care
March 5, 2025Ambulatory care clinics are under growing pressure to do more with less—managing high patient volumes, maintaining compliance, and ensuring seamless care coordination.
However, a major roadblock stands in the way: disconnected systems that force providers and staff to waste valuable time on manual data entry, redundant processes, and workarounds.
Without interoperability in ambulatory care, EHRs, billing platforms, telehealth services, and patient engagement tools remain siloed, creating staffing inefficiencies, administrative burdens, and financial strain. Clinicians struggle with incomplete patient data, prior authorizations get delayed, and revenue cycle management becomes a constant challenge.
At John Lynch & Associates, we specialize in helping ambulatory care leaders navigate these challenges by optimizing health IT systems, ensuring regulatory compliance, and driving operational efficiency.
Our expertise in EHR integration, workflow automation, and interoperability strategies empowers clinics to reduce administrative burdens and improve patient outcomes.
The solution? A strategic approach to interoperability that breaks down data silos, automates workflows, and ensures compliance with evolving regulations. This article explores how interoperability addresses staffing and operational challenges, providing ambulatory care leaders with the insights needed to navigate this critical transformation.
What is the Role of Interoperability in Ambulatory Care Clinics?
Interoperability Enhances Coordination and Efficiency Across Systems
Ambulatory care clinics rely on multiple digital tools—EHRs, billing systems, telehealth platforms, and patient engagement solutions—to manage clinical and administrative tasks. However, when these systems operate in isolation, inefficiencies arise, leading to data silos, redundant workflows, and communication breakdowns between providers, staff, and patients.
Interoperability bridges these gaps by enabling seamless data exchange between disparate systems. By ensuring that patient records, billing data, and scheduling information flow freely across platforms, clinics can:
- Enhance care coordination by providing clinicians with complete, real-time patient data.
- Reduce manual effort by automating administrative workflows and minimizing duplicate data entry.
- Improve patient experiences by enabling seamless interactions across appointment scheduling, telehealth visits, and follow-up care.
Example:
In ambulatory care, EHR interoperability in healthcare often hinges on the central role of EHR systems. Without interoperability, these systems remain isolated, forcing staff to toggle between platforms, re-enter information manually, and rely on outdated data—delaying care and frustrating both patients and providers.
By implementing interoperable health IT solutions, clinics can eliminate these inefficiencies and set the foundation for streamlined, patient-centered care.
Why Are Health IT Standards a Precursor to Interoperability?
IT Standards Ensure Compatibility and Simplify Data Exchange
For interoperability to function effectively, ambulatory care clinics must adopt standardized protocols that enable different systems to communicate seamlessly. Without a universal framework, EHRs, billing platforms, and patient portals operate in silos, leading to incompatible data formats, delayed information sharing, and inefficiencies that burden staff and providers.
Key health IT standards like FHIR (Fast Healthcare Interoperability Resources) and HL7 (Health Level Seven) serve as the foundation for interoperability by:
- Ensuring system compatibility across different vendors and platforms.
- Facilitating seamless data exchange between EHRs, billing systems, and payer networks.
- Supporting regulatory compliance with federal mandates for data sharing and transparency.
Compliance Connection:
Regulatory requirements continue to push the industry toward greater interoperability. The CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) mandates that healthcare payers implement FHIR-based APIs to streamline prior authorization requests. Clinics that align with these standards can reduce administrative burdens, improve approval times, and enhance compliance with evolving regulations.
Example:
Adopting EHR solutions for outpatient clinics that comply with FHIR and HL7 ensures that critical data—such as patient histories, lab results, and billing details—can be exchanged instantly between systems. Without these standards, clinics face integration roadblocks, delayed reimbursements, and inefficient workflows that negatively impact patient care.
Challenges Ambulatory Care Clinics Face with FHIR & HL7 Adoption
Ambulatory care clinics often struggle with adopting FHIR (Fast Healthcare Interoperability Resources) and HL7-compliant systems due to:
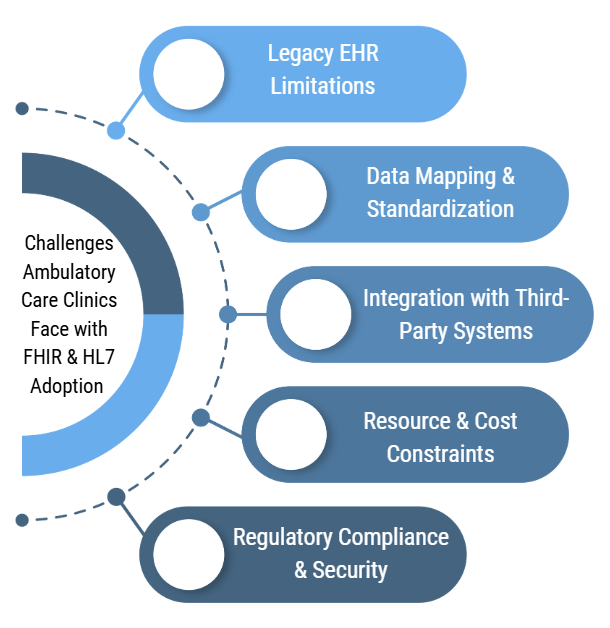
- Legacy EHR Limitations – Many clinics operate on outdated EHR systems that lack seamless interoperability with FHIR-based applications.
- Data Mapping & Standardization – Converting existing data to HL7-compliant formats can be complex, requiring extensive mapping and validation.
- Integration with Third-Party Systems – Connecting to payers, HIEs, and external health systems often involves complex API configurations and compliance hurdles.
- Resource & Cost Constraints – Smaller clinics lack the IT resources and budget to manage full-scale FHIR implementations.
- Regulatory Compliance & Security – Ensuring adherence to HIPAA, CMS regulations, and FHIR security protocols requires expertise in both compliance and IT.
How John Lynch & Associates Has Helped Clinics Overcome These Challenges
Our team has worked with ambulatory care clinics to simplify FHIR & HL7 adoption by:
✅ Assessing EHR compatibility and recommending cost-effective integration strategies
✅ Developing standardized data mapping to align clinic workflows with HL7 guidelines
✅ Implementing API-based solutions for seamless interoperability with external systems
✅ Providing compliance guidance to ensure secure data exchange under HIPAA & CMS regulations
✅ Training staff on FHIR/HL7 workflows to optimize data accuracy and operational efficiency
Case Study: Enabling HL7 Integration for a Multi-Specialty Ambulatory Clinic
A multi-specialty ambulatory care clinic in the Southwest needed to connect their EHR with a regional HIE to improve care coordination and meet new CMS interoperability mandates. However, their existing EHR lacked native FHIR support, making direct integration difficult.
Our Solution:
- Conducted a gap analysis to identify key interoperability challenges
- Partnered with a middleware vendor to enable HL7/FHIR data exchange without replacing the entire EHR
- Mapped key clinical data elements (e.g., demographics, lab results, and visit summaries) to HL7 standards
- Implemented real-time API connections to sync data between the EHR, HIE, and external provider networks
- Trained staff on FHIR-based workflows to improve data consistency and compliance
Impact & Outcomes:
✅ 95% reduction in manual data entry through automated interoperability
✅ Faster referrals & information sharing, reducing administrative delays by 50%
✅ 100% compliance with CMS interoperability requirements
✅ Avoided costly EHR replacement, saving the clinic $250K+ in upgrade costs
By enabling FHIR & HL7 integration without disrupting daily operations, our team helped the clinic improve care coordination, reduce administrative burden, and meet regulatory requirements efficiently.

How Does Interoperability Reduce Administrative Burdens in Ambulatory Care?
Automation Simplifies Workflows and Reduces Manual Tasks
Administrative inefficiencies are one of the biggest challenges in ambulatory care. From prior authorizations and patient scheduling to billing and claims processing, manual processes create bottlenecks that slow down operations, increase labor costs, and contribute to staff burnout. Interoperability reduces these burdens by automating workflows and enabling seamless communication between systems.
By integrating APIs (Application Programming Interfaces) and automated data exchange, interoperable systems allow clinics to:
- Eliminate redundant data entry by ensuring patient records update automatically across platforms.
- Accelerate prior authorization approvals by allowing EHRs to submit requests directly to payers.
- Reduce billing errors by aligning clinical documentation with payer requirements, decreasing claim denials.
Example:
An interoperable EHR can automatically submit prior authorization requests through payer APIs, eliminating the need for staff to manually re-enter data across different platforms. This not only reduces administrative strain but also shortens approval times, ensuring patients receive the care they need without unnecessary delays.
John Lynch & Associates Perspective:
Ambulatory care clinics often face operational inefficiencies due to time-consuming administrative tasks that hinder productivity and patient care. Staff spend hours on manual data entry and duplicate documentation, inputting patient demographics, visit summaries, and insurance details across multiple systems.
Prior authorizations and claims processing further slow operations, as manual submissions and tracking delays patient care and disrupt revenue flow. Scheduling and patient communication require extensive administrative effort to coordinate appointments, reminders, and follow-ups efficiently.
Additionally, interoperability gaps and data retrieval pose significant challenges, as outdated EHR systems make it difficult to exchange patient data with hospitals, specialists, and payers. Lastly, regulatory compliance and reporting consume valuable time, with clinics needing to meet stringent CMS, AHCCCS, and HIPAA documentation requirements through labor-intensive audits and reporting processes.
Our team has helped ambulatory care clinics overcome these challenges by implementing HL7/FHIR-based interoperability to automate EHR data entry and exchange, eliminating duplicate documentation and streamlining workflows.
We have also optimized prior authorizations by integrating real-time eligibility verification and electronic authorization tools, significantly reducing approval times.
To enhance scheduling and patient outreach, we implemented AI-driven scheduling systems that minimize no-shows and improve patient engagement. Additionally, we have automated compliance reporting with advanced tracking tools, ensuring clinics adhere to CMS, AHCCCS, and HIPAA requirements without the burden of manual audits.
Lastly, we have integrated RCM and billing workflows, improving data accuracy and automating claims submissions to reduce denials and accelerate reimbursements.
By leveraging interoperability to streamline workflows and reduce administrative burdens, ambulatory care clinics can increase staff efficiency, reduce costs, and enhance patient care delivery.
What is the Financial Impact of Interoperability on Clinics?
Interoperability Improves Cash Flow and Boosts ROI
Beyond improving workflows, interoperability directly impacts a clinic’s financial health by reducing errors, expediting reimbursements, and optimizing revenue cycle management. Disconnected systems often lead to billing discrepancies, claim denials, and delays in payment processing—ultimately affecting cash flow.
By integrating EHRs, billing systems, and payer networks, interoperable solutions help clinics:
- Reduce claim denials by ensuring billing data is accurate, complete, and aligned with payer requirements.
- Improve reimbursement timelines by enabling real-time data exchange between providers and payers.
- Optimize resource allocation by minimizing the administrative burden of manual billing corrections.
Example:
Clinics that implemented interoperable EHR and billing systems reported a 20% reduction in claim denials and a 15% improvement in collection times, resulting in stronger cash flow and significant cost savings. By reducing manual intervention in the revenue cycle, clinics can focus resources on patient care rather than chasing reimbursements.
By leveraging AI-driven EHR systems to streamline billing workflows and improve claims processing, clinics can reduce administrative burdens and accelerate reimbursement timelines—creating a more predictable revenue cycle.
By investing in interoperability for ambulatory care, clinics can minimize financial risk, enhance revenue cycle efficiency, and achieve sustainable financial growth.
How Can Ambulatory Care Leaders Prepare for Interoperability?
Strategic Planning and Investment Drive Interoperability Success
Achieving interoperability isn’t just about adopting new technology—it requires a strategic approach to IT infrastructure, process optimization, and staff readiness. Ambulatory care leaders must ensure their systems are scalable, compliant, and seamlessly integrated to maximize efficiency and patient care.
To successfully implement interoperability, clinics should focus on three key steps:
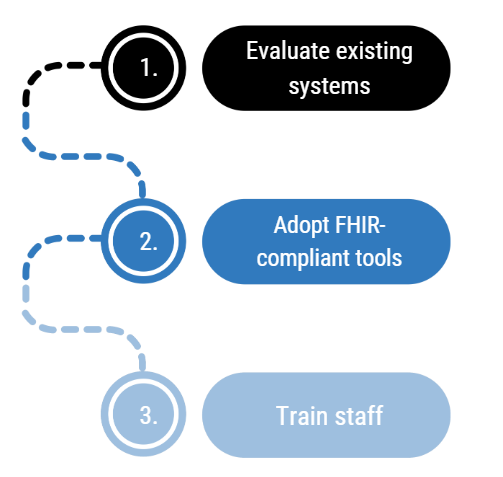
- Evaluate existing systems: Identify gaps where data silos, inefficient workflows, or compliance risks hinder operational performance.
- Adopt FHIR-compliant tools: Ensure EHRs, billing platforms, and patient portals adhere to modern interoperability standards for seamless integration.
- Train staff: Equip teams with the knowledge and resources needed to effectively utilize interoperable systems and maximize their benefits.
Example:
A clinic transitioning to an interoperable EHR system saw immediate improvements in care coordination and administrative efficiency. By integrating FHIR-based APIs, they eliminated duplicate data entry, reduced manual scheduling errors, and expedited prior authorizations—freeing staff to focus on higher-value patient interactions.
John Lynch & Associates Perspective:
During audits of ambulatory care IT systems, we have identified several common gaps that hinder efficiency, security, and compliance. Many clinics struggle with EHR interoperability issues, where outdated systems lack seamless data exchange with external providers, payers, and Health Information Exchanges (HIEs).
Inadequate cybersecurity measures are another frequent concern, with weak access controls, insufficient data encryption, and a lack of regular security assessments leaving patient data vulnerable to breaches.
Additionally, manual and inefficient billing processes contribute to revenue cycle inefficiencies, leading to increased claim denials and delays in reimbursements.
We also find gaps in compliance readiness, where clinics fail to meet evolving CMS, AHCCCS, and HIPAA requirements due to inadequate audit trails and inconsistent documentation practices.
Lastly, limited IT infrastructure support and a lack of staff training on system optimization prevent clinics from fully leveraging their technology, further impacting operational stability and patient care quality.
By investing in interoperability solutions tailored to their unique needs, ambulatory care leaders can future-proof their operations, reduce administrative burdens, and drive long-term success.

Interoperability is the Future of Ambulatory Care
The demands on ambulatory care clinics are increasing, and interoperability is no longer optional—it’s essential for efficient, compliant, and patient-centered care. By eliminating data silos, automating administrative workflows, and streamlining revenue cycle management, interoperability directly addresses the staffing and operational challenges clinics face daily.
Regulatory requirements and health IT advancements continue to drive the industry forward, making it critical for clinics to adopt scalable, standards-based interoperability solutions. As highlighted in Forbes’ top healthcare trends, seamless data exchange and automation will play a key role in shaping the future of outpatient care.
By strategically implementing FHIR-compliant EHR systems, payer APIs, and automated workflows, clinics can reduce administrative burdens, improve financial performance, and enhance patient outcomes—positioning themselves for long-term success.
Ready to unlock the power of interoperability? Contact John Lynch & Associates today to learn how our IT consulting services can help your ambulatory care clinic achieve seamless data integration and operational excellence.
