
Revenue Integrity in Healthcare: What It Means for Tribal Health Organizations
April 16, 2025Revenue integrity is the foundation of financial sustainability in healthcare. It ensures that every service provided is accurately documented, coded, and reimbursed—without errors, compliance risks, or revenue loss. But for Tribal health organizations, maintaining revenue integrity in healthcare comes with unique challenges.
With a complex mix of Indian Health Service (IHS) funding, third-party reimbursements, and federal-tribal regulations, Tribal health leaders must navigate a system that is vastly different from traditional healthcare settings. Billing errors, denied claims, and compliance gaps can lead to significant revenue leakage, jeopardizing both financial health and patient care quality.
At John Lynch & Associates, we understand these challenges. Our expertise in tribal health revenue cycle management (RCM) helps healthcare organizations optimize billing accuracy, reimbursement strategies, and compliance processes to strengthen financial sustainability.
In this article, we explore:
- What revenue integrity means for Tribal health organizations?
- Common revenue risks, including billing errors and compliance challenges.
- Best practices to reduce claim denials and prevent revenue leakage.
- How to improve financial sustainability without compromising patient care.
By taking a proactive approach to revenue integrity in Tribal healthcare, organizations can not only maximize reimbursements but also ensure long-term financial stability—empowering them to continue delivering high-quality, culturally competent care to their communities.
Understanding Revenue Integrity in Tribal Health
Defining Revenue Integrity
At its core, revenue integrity in healthcare is about ensuring that the clinical services provided to patients are properly documented, accurately coded, and fully reimbursed. It bridges the gap between care delivery and financial operations—aligning patient services, coding, billing, and compliance into a single, cohesive process.
For Tribal health organizations, revenue integrity is more than just a financial concern. It’s a strategic necessity. Without it, even well-run clinics can experience significant revenue loss due to inaccurate claims, delayed payments, or regulatory penalties. Strong revenue integrity practices help safeguard resources essential to providing reliable, high-quality care in Tribal communities.
Unique Financial Challenges in Tribal Healthcare
Unlike many non-Tribal healthcare systems, Tribal health organizations often operate under a layered and nuanced financial model. Funding typically comes from a combination of:

Each of these streams comes with its own regulations, requirements, and risks. For instance, while IHS provides foundational funding, it does not always cover the full cost of services, particularly for tribally operated programs. This makes third-party reimbursements essential to closing funding gaps—but navigating these reimbursements can be especially complex without a robust revenue integrity framework.
One key financial factor for tribally operated health programs is Contract Support Costs (CSCs)—funding that helps cover administrative overhead, including billing and compliance operations. The recent U.S. Supreme Court decision in Becerra v. San Carlos Apache Tribe has major implications for CSC reimbursements and Tribal autonomy in managing health programs.
Understanding and optimizing these funding streams is key to effective revenue integrity in tribal health—but without the right systems and expertise in place, revenue can easily fall through the cracks.
Revenue Integrity in Action
A Tribal health clinic in the Western U.S. serving 3,500 community members faced a growing problem: rising patient visits, but declining revenue. Despite IHS and Medicaid funding, they struggled with a 23% denial rate, unbilled encounters, compliance gaps, and credentialing delays—all impacting patient care and financial health.
John Lynch & Associates conducted a full revenue integrity audit and implemented tailored solutions, including:
- Custom coding guides and documentation tools
- A culturally aligned compliance program
- Streamlined workflows and credentialing processes
In just 90 days, results included:
- Denials reduced from 23% to 7%
- Revenue jumped from $115K to $160K/month
- Unbilled encounters dropped by over 90%
- Staff training and compliance rates hit 100%
With improved financial performance and operational efficiency, the clinic is now expanding into mobile outreach and new services.
Read the full case study here.

Common Revenue Integrity Risks in Tribal Health Organizations
Maintaining revenue integrity in tribal healthcare requires constant vigilance. From front-desk registration to final claim submission, even small errors can lead to denied claims, lost revenue, and compliance exposure. Unfortunately, these issues often go unnoticed until they start affecting financial performance and patient care delivery.
Billing Errors and Revenue Leakage
One of the most frequent threats to revenue integrity is billing inaccuracy. In many Tribal health clinics, front-to-back revenue cycle workflows can become fragmented—especially when teams are stretched thin, or staff turnover is high.
Common issues include:
- Incorrect or incomplete coding
- Inconsistent use of modifiers
- Unbilled encounters due to missing documentation
- Duplicate or delayed claims from breakdowns in communication between departments
These errors create revenue leakage—preventable losses that slowly drain financial resources. Without a structured review process in place, clinics may not realize the scale of missed revenue opportunities.
For a closer look at how billing mistakes can undermine financial health, see our guide:
Common Billing Errors in Tribal Healthcare and How to Avoid Them
Compliance and Regulatory Challenges
Tribal health organizations operate under a unique regulatory environment, balancing requirements from IHS, CMS, state Medicaid programs, and Tribal governance. That complexity increases the risk of falling out of compliance—especially when regulations change, or staffing is inconsistent.
Some of the most pressing compliance risks include:
- Outdated policies and procedures
- Improper documentation for IHS and Medicaid claims
- Missing or delayed provider credentialing
- Limited internal auditing or staff training
Beyond the financial penalties, compliance issues can lead to audit fatigue, reputational harm, and—in some cases—interruption of services.
The Cost of Poor Revenue Integrity – Data & Impact
The financial cost of weak revenue integrity isn’t always obvious—but it adds up quickly. Consider the following national and Tribal-specific data points:
- Claim denial rates in healthcare average between 6–13%, but some Tribal clinics experience rates above 20%.
- Billing errors can cost up to $17 per claim in rework and follow-up.
- For clinics operating under IHS or 638 compacts, even small gaps in third-party reimbursement can account for hundreds of thousands in lost annual revenue.
- A 2023 audit of a tribally operated facility revealed over 300 unbilled encounters in a six-month period—simply due to missing documentation.
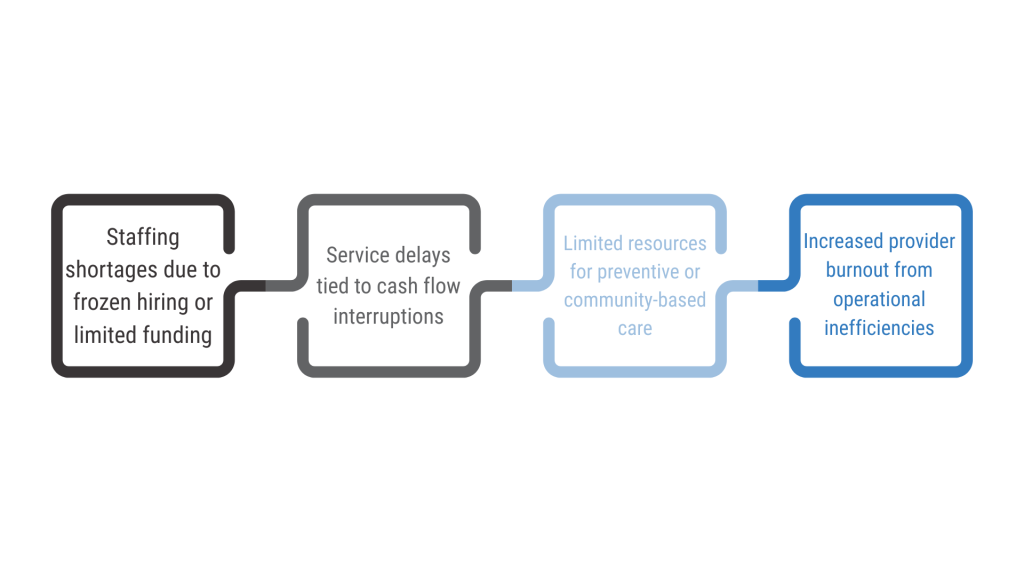
Poor revenue integrity also contributes to:
- Delayed hiring or provider turnover
- Reduced availability of culturally appropriate care services
- Inability to invest in technology or community outreach programs
These risks aren’t just financial—they’re deeply operational, often affecting how well a clinic can serve its community today and plan for tomorrow.
RCM Strategies for Indian Health Service Providers
Achieving strong revenue integrity in tribal health isn’t about avoiding errors—it’s about building a proactive, sustainable approach to revenue cycle management. By aligning people, processes, and technology, Tribal health organizations can increase reimbursements, reduce denials, and maintain compliance across funding sources.
Best Practices for Improving Revenue Integrity in Tribal Healthcare
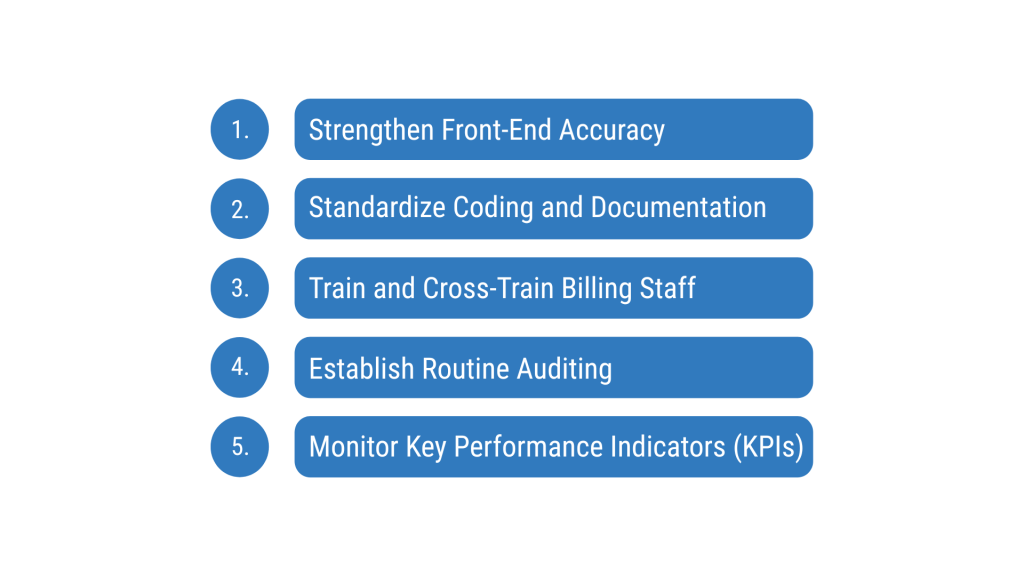
Here are foundational RCM strategies for Indian Health Service providers and Tribal clinics seeking to strengthen revenue integrity:
1. Strengthen Front-End Accuracy
Revenue integrity starts the moment a patient is registered. Ensuring complete and accurate data collection—such as insurance verification, proper encounter types, and demographics—helps prevent downstream issues.
2. Standardize Coding and Documentation
Use custom coding guides tailored to Tribal and behavioral health services. Provide real-time documentation checklists for providers to ensure consistency. This helps minimize denials due to missing or vague information.
3. Train and Cross-Train Billing Staff
With frequent staff turnover in Tribal health systems, ongoing training is essential. Crosstrain staff on both clinical and billing systems to reduce silos and ensure smooth handoffs between departments.
4. Establish Routine Auditing
Implement regular internal audits to identify billing gaps, compliance risks, and training needs. These audits help build a culture of accountability and continuous improvement.
5. Monitor Key Performance Indicators (KPIs)
Track metrics like denial rates, days in A/R, unbilled encounters, and first pass claim acceptance rates. These KPIs serve as early warning signs for revenue cycle breakdowns.
Leveraging Third-Party Reimbursement Strategies
Many Tribal health clinics depend on third-party revenue—often from Medicaid, Medicare, and private payers—to supplement IHS base funding. However, securing full reimbursement requires strategic planning and deep understanding of payer requirements.
To strengthen third-party reimbursement:
- Stay current with Medicaid billing rules, especially state-specific requirements that may differ from IHS standards.
- Negotiate payment terms and follow-up timelines with private payers to ensure accountability.
- Use denial trend reports to identify recurring payer issues and escalate as needed.
- Ensure that credentialing workflows are in place to avoid delays in billing for newly hired providers.
Technology and Automation in Revenue Integrity
Investing in technology isn’t about replacing staff—it’s about empowering them with tools that reduce error and streamline processes. Tribal clinics increasingly rely on EHR-integrated revenue cycle tools to strengthen performance.
Effective technology solutions include:
- Real-time alerts for incomplete encounters or missing documentation
- Automated coding support and modifier checks
- Analytics dashboards that flag underperforming areas
- Credentialing tracking systems to prevent billing under unenrolled providers
These tools not only improve accuracy but also free up staff to focus on high-value tasks like patient engagement and care coordination. Clinics that embrace automation and analytics often see faster reimbursement cycles, reduced billing errors, and improved cash flow—key indicators of strong revenue integrity.
Strengthening Financial Sustainability Without Compromising Care
Revenue integrity isn’t just a finance issue—it’s a care issue. When Tribal health organizations lose revenue due to claim denials, compliance lapses, or billing delays, the downstream effects are felt by patients, providers, and the broader community.
The Link Between Revenue Integrity and Patient Care
Every dollar lost to inefficiency or error is a dollar that could have gone toward improving care access, investing in cultural programming, or expanding services like dental, behavioral health, or mobile outreach.
Common consequences of poor revenue integrity include:
In contrast, clinics that prioritize revenue integrity can reinvest in areas that directly benefit the community—without compromising their cultural mission or clinical quality.
When Tribal health organizations achieve financial stability, they are better positioned to:
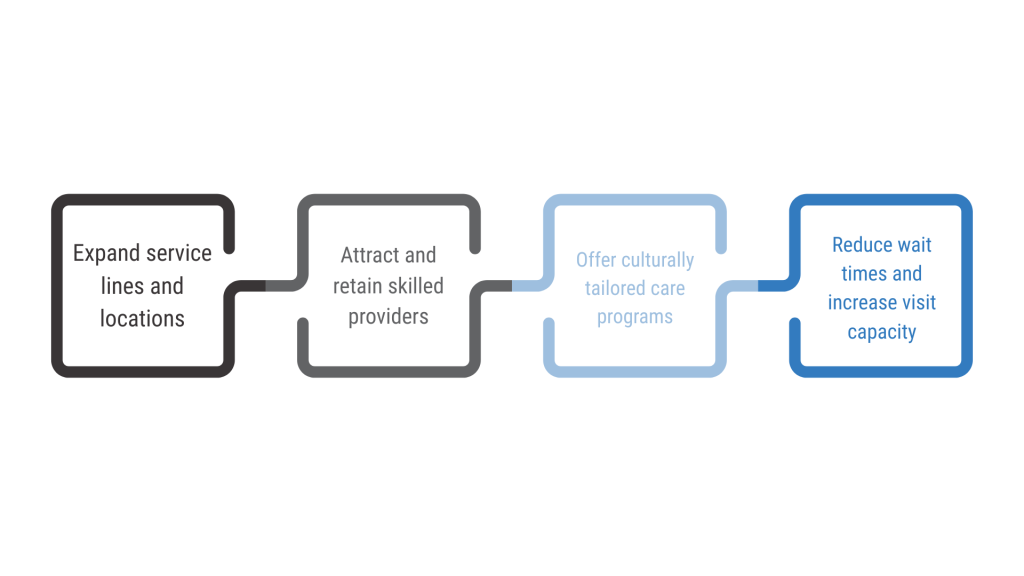
Revenue integrity, in this context, becomes a means to preserve sovereignty, improve care, and strengthen community well-being.
Long-Term Financial Sustainability Strategies
Sustaining improvements in revenue integrity requires more than a one-time fix. It calls for a long-term strategy that integrates people, processes, and technology with the unique operational needs of Tribal health systems.
Key sustainability strategies include:
- Ongoing staff education on evolving payer requirements and compliance standards
- Quarterly internal audits to monitor billing performance and catch emerging issues early
- Investments in EHR optimization and data analytics to support proactive decision-making
- Credentialing workflows to avoid billing interruptions and provider enrollment delays
- Partnerships with revenue cycle experts who understand the cultural, clinical, and regulatory environment of Tribal healthcare
With the right foundation, Tribal health clinics can build resilience—not just in their finances, but across their entire system of care.

Conclusion
Revenue integrity in healthcare is more than a technical goal—it’s a vital part of ensuring that Tribal health organizations remain financially stable, compliant, and prepared to meet the evolving needs of their communities.
For Tribal clinics, the stakes are high. With limited IHS funding and increasing reliance on third-party payers, even small gaps in billing accuracy or compliance can lead to significant financial loss. But with the right strategies—rooted in cultural respect, operational efficiency, and data-driven practices—Tribal health systems can protect their revenue while advancing their mission of holistic, community-centered care.
At John Lynch & Associates, we understand the nuances of revenue integrity in tribal health. Our tailored solutions help Tribal organizations implement sustainable, compliant, and culturally aligned RCM strategies that make a measurable difference.
If you’re a Tribal health leader concerned about revenue leakage, claim denials, or compliance challenges, now is the time to act.
Let’s work together to build a stronger revenue foundation—one that supports both your mission and your community.
Contact John Lynch & Associates to schedule a revenue integrity assessment or learn more about our Tribal health consulting services.
References & Further Reading
- Indian Health Service – About IHS
Overview of the IHS mission, services, and the role it plays in Tribal health delivery. - IHS – Implementation of Supreme Court Decision: Becerra v. San Carlos Apache Tribe
Details on how IHS is addressing contract support costs following the Supreme Court ruling. - Common Billing Errors in Tribal Healthcare and How to Avoid Them
Insight from John Lynch & Associates on billing risks and how Tribal clinics can improve accuracy. - Healthcare Compliance Challenges in Tribal Health Facilities
A breakdown of common compliance pitfalls in Tribal healthcare and how to mitigate them. - CASE STUDY: Improving Revenue Integrity for a Tribal Health Clinic Background
