Audit season doesn’t come with a warning sign. For behavioral health organizations, readiness is no longer about scrambling before a scheduled review, it’s about being prepared all the time. And at the center of that responsibility is the compliance officer.
Often operating behind the scenes, compliance leaders shoulder a complex burden: navigating evolving regulations, translating policies into practice, and keeping teams aligned across clinical, billing, and administrative functions. When audit risk rises (and it is rising) compliance officers are expected to not only respond, but to anticipate.
With increased scrutiny from payers, the Office for Civil Rights (OCR), and CMS, behavioral health organizations are facing higher stakes in every aspect of care delivery and documentation. Recent HIPAA enforcement actions show that even well-meaning teams can fall short when audit readiness is treated as a checkbox instead of a culture.
This article explores the evolving role of the compliance officer in today’s behavioral health environment. We’ll examine where audits are focusing now, what proactive preparation really looks like, and how compliance leaders can shift from enforcers to strategic partners; ensuring that audit readiness is woven into the very fabric of care.
- 1. Why Audit Readiness Remains a Pressing Priority for Behavioral Health Compliance Leaders
- 2. What Today’s Audit Environment Looks Like in Behavioral Health
- 3. Building a Culture That Supports Continuous Audit Readiness
- 4. Practical Steps to Strengthen Your Audit Readiness Framework
- 5. The Compliance Officer as Strategic Collaborator and Change Leader
- 6. Audit Readiness Is an Ongoing Practice (Not a One-Time Event)
- 7. Further Reading
- 8. Related Articles
- Audits in behavioral health are increasing in scope, documentation, supervision, and telehealth use are all under review.
- Effective compliance officers drive readiness by building shared ownership, not fear-based accountability.
- Real audit preparedness comes from integrated systems, internal walkthroughs, and continuous staff education not last-minute fixes.
Why Audit Readiness Remains a Pressing Priority for Behavioral Health Compliance Leaders
The phrase "audit readiness" might sound procedural, but in behavioral health, it’s deeply personal. Behind every compliance checklist is a team trying to do right by their clients, protect their organization, and uphold the standards that make quality care possible. That’s what makes the compliance officer’s role so unique and so complex.
Behavioral Health Under the Microscope
Behavioral health organizations are experiencing a notable shift in regulatory oversight. What once felt like a lower-risk corner of healthcare is now squarely in focus for auditors and enforcement agencies. The scrutiny is wide-ranging - spanning documentation, billing accuracy, service delivery, privacy practices, and the use of telehealth.
Oversight bodies and payers are ramping up in several key areas:
- CMS is taking a closer look at billing patterns and clinical appropriateness.
- Medicaid agencies are requiring more nuanced, real-time documentation.
- The Office for Civil Rights (OCR) is intensifying its investigations into data privacy and breach protocols.
- Private insurers are flagging telehealth records for inconsistencies in consent and treatment validation.
The message is clear: no matter the size or specialization of the behavioral health organization, strong compliance practices are expected.
Pressure from All Sides: The Unique Role of the Compliance Officer
Unlike roles confined to one department, compliance officers operate across the entire organization. You’re expected to:
- Translate legal and regulatory language into actionable internal policies
- Monitor daily workflows you don’t directly manage
- Influence executive decisions while gaining staff buy-in
- Respond swiftly to issues without eroding trust
It’s a position that demands not only technical knowledge, but also diplomacy, consistency, and foresight.
Beyond Pass/Fail: Reframing Audits as a Measure of Integrity and Preparedness
Too often, audit readiness is treated like a fire drill; stressful, urgent, and short-lived. But the best-prepared organizations understand that audits aren’t just about passing. They’re an opportunity to:
- Identify weak spots before they become liabilities
- Validate the organization’s commitment to ethical, person-centered care
- Strengthen cross-functional alignment and communication
When readiness becomes part of the culture, not just a compliance function, everyone benefits.

What Today’s Audit Environment Looks Like in Behavioral Health
Audit readiness starts with one question: would your current systems hold up if someone were reviewing them today? Understanding what auditors actually look for, and how small gaps become big risks, is what separates reactive organizations from prepared ones.
Common Areas of Scrutiny
Common telehealth compliance risks include:
- Missing or inconsistent documentation of time, modality (audio vs. video), and patient consent
- Billing for services that lack medical necessity under virtual conditions
- Using incorrect place-of-service or modifier codes
- Incomplete credentialing or supervision protocols for virtual providers
These may sound like technical issues, but collectively they pose a serious compliance risk—particularly when multiplied across hundreds or thousands of claims.
Red Flags That Often Trigger Audits
Most audits don’t happen randomly. They’re often prompted by patterns or signals that suggest risk, including:
- Frequent corrections or resubmissions on claims
- High staff turnover with insufficient training handoffs
- Inconsistent EHR documentation across providers or programs
- Use of outdated paper forms or templates not aligned with current billing codes
- Client complaints or reports to regulatory bodies
In many cases, these indicators aren’t visible until it’s too late - when the audit has already begun. Organizations that struggle with fragmented workflows, siloed teams, or outdated procedures are often vulnerable to the kinds of compliance threats that quietly build over time and later trigger high-stakes reviews.
Building a Culture That Supports Continuous Audit Readiness
Audit readiness isn’t something that can be delegated to one role or achieved through one training. It’s a reflection of the organization’s daily habits, communication norms, and shared understanding of accountability. For compliance officers, this means shifting the conversation from isolated requirements to collective responsibility.
Move from Policy to Practice
Most behavioral health teams don’t lack policies. What they often lack is clarity on how those policies show up in real-world situations. Are staff trained on how to document supervision? Do clinicians understand the rationale behind signature requirements or service authorization timeframes?
When compliance guidance feels abstract, it gets overlooked. When it’s grounded in daily practice, it becomes second nature.
Strengthen Ownership Without Creating Fear
One of the biggest barriers to a readiness-focused culture is the perception that compliance is punitive. If staff worry they’ll be blamed for errors, they’re less likely to raise concerns or ask clarifying questions.
Instead, audit readiness should be framed as a shared safeguard; something that protects clients, supports ethical care, and reduces stress when reviews happen. Reinforcing that message regularly helps build a culture of openness, not avoidance.
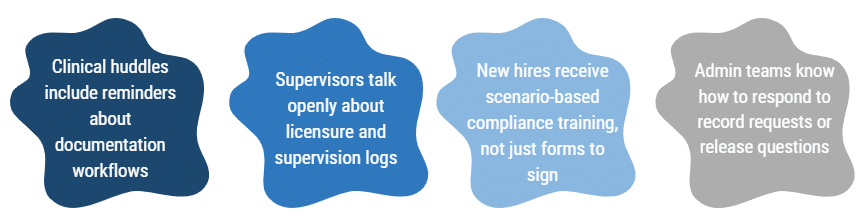
Normalize Compliance Conversations Across Teams
Compliance can’t live in a silo. Organizations that stay audit-ready tend to make policy conversations part of routine operations:
When compliance is woven into how people work and not just what they’re told, it becomes part of the culture, not a burden on top of it.
Practical Steps to Strengthen Your Audit Readiness Framework
Audit readiness can feel abstract until the request for records arrives. At that point, the question isn’t whether your team is committed to compliance, but whether your systems make it easy to demonstrate. For compliance officers, the goal is to build structures that prevent last-minute scrambles and reduce risk long before an audit is triggered.
How to Be Ready for an Audit
Being ready for an audit means more than having policies on file or records stored. It’s about being able to demonstrate, clearly and quickly, that your organization operates in alignment with regulatory expectations.
To be audit-ready at any time, behavioral health organizations should:
- Ensure documentation is complete, timely, and aligned with services billed
- Maintain up-to-date supervision logs and staff credentialing records
- Verify that telehealth services include proper consent and location compliance
- Train staff regularly on documentation, privacy, and record retention
- Run internal audit simulations to uncover and fix gaps
- Track compliance metrics using real-time data, not just static checklists
Readiness is not about perfection, it’s about systems that support consistency and transparency, even in day-to-day operations.
Run Internal Walkthroughs - Not Just Audits
Formal internal audits are valuable, but they often focus on outcomes. To uncover weak spots in real time, try walkthroughs: informal exercises where staff simulate responding to an actual audit. Ask questions like:
- Can clinical staff locate a supervision log without assistance?
- Do admin teams know where the most recent policy versions are stored?
- What happens when a client requests a copy of their records?
These drills not only surface documentation or access issues but also help normalize audit preparedness as part of regular operations.
Build a Living Compliance Playbook
Many organizations rely on a patchwork of PDF policies, binders, and verbal guidance that’s hard to navigate, and even harder to keep current. A living compliance playbook is centralized, searchable, and accessible across departments.
It should include:
- Clear definitions of compliance responsibilities by role
- Links to up-to-date forms, procedures, and workflows
- Real-world examples and FAQs to support staff judgment
- A documented review and version history
When staff don’t have to guess what “compliant” looks like, they’re far more likely to follow through.
Leverage Technology to Spot Risks Early
EHRs, billing software, and quality dashboards can all support audit readiness if they’re used intentionally. But tech is not a substitute for oversight.
- Set up alerts for incomplete documentation or unsigned notes
- Run periodic reports on supervision records or license expirations
- Track staff training completion and exceptions
These small checks, done routinely, can prevent bigger issues from surfacing during an external review.
Organizations that excel in audit readiness tend to invest in systems designed for sustainability. That includes thoughtful audit planning, cross-functional coordination, and tailored support structures that reflect the realities of behavioral health. These are the kinds of strategies we help leaders put into place through our audit preparation and support work; built around collaboration, not just checklists.

The Compliance Officer as Strategic Collaborator and Change Leader
In many behavioral health organizations, compliance officers are seen as the people who say “no” - the policy gatekeepers, the audit overseers, the ones who surface problems that others would rather avoid. But the reality is more nuanced: effective compliance leaders aren’t just enforcing rules; they’re building trust, bridging departments, and shaping a culture that prioritizes quality care.
From Enforcer to Educator
When compliance is framed solely around restriction, it’s easy for teams to disengage, or view it as someone else’s job. But when compliance officers step into an educator role, the dynamic shifts. Staff are more likely to ask questions, own their responsibilities, and treat compliance as part of client care and not a parallel system.
That shift starts with how compliance leaders show up: Are they available? Do they explain the “why” behind the policy? Do they provide tools that support, rather than complicate, daily work?
Partnering Across Departments
Audit readiness doesn’t live in a single department. It’s shaped by how clinical, billing, HR, and administrative teams operate together. Compliance officers who collaborate early, when forms are created, workflows are updated, or staffing models shift, can prevent risks before they become audit findings.
That kind of partnership takes intention. It means being in the room where program decisions are made. It means translating policy into practical support, not just documentation. And it means advocating for resources that protect both the organization and the people it serves.
Making the Case Without Fear-Based Tactics
Audit findings and compliance breakdowns carry real consequences, but leading through fear rarely builds sustainable change. Instead, the most effective compliance officers make the case for readiness by aligning with the organization’s values:
- Protecting the client experience
- Safeguarding staff and licensure
- Improving organizational resilience
- Reducing financial and legal exposure
In this way, audit readiness becomes part of the organization's long-term vision—not just a reaction to risk.
Audit Readiness Is an Ongoing Practice (Not a One-Time Event)
In many behavioral health organizations, compliance officers are seen as the people who say “no” - the policy gatekeepers, the audit overseers, the ones who surface problems that others would rather avoid. But the reality is more nuanced: effective compliance leaders aren’t just enforcing rules; they’re building trust, bridging departments, and shaping a culture that prioritizes quality care.
Ready to Talk?
Further Reading
John Lynch & Associates
- Compliance Risk in Healthcare: 7 Emerging Threats to Watch: An insight article exploring system-wide compliance vulnerabilities, including documentation gaps, audit triggers, and operational blind spots.
U.S. Department of Health & Human Services (OIG)
-
HIPAA Enforcement Highlights: September 2024: A summary of recent HIPAA enforcement actions, illustrating common compliance pitfalls in privacy, security, and risk assessment.