- 1. What Is Compliance Risk in Healthcare?
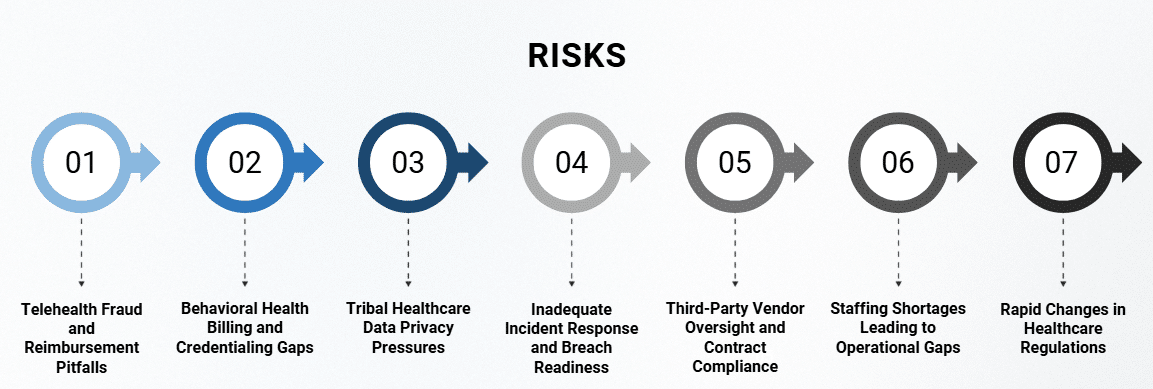
- 2. Risk #1 – Telehealth Fraud and Reimbursement Pitfalls
- 3. Risk #2 – Behavioral Health Billing and Credentialing Gaps
- 4. Risk #3 – Tribal Healthcare Data Privacy Pressures
- 5. Risk #4 – Inadequate Incident Response and Breach Readiness
- 6. Risk #5 – Third-Party Vendor Oversight and Contract Compliance
- 7. Risk #6 – Staffing Shortages Leading to Operational Gaps
- 8. Risk #7 – Rapid Changes in Healthcare Regulations
- 9. Building a Future-Ready Compliance Strategy
- 10. Turning Compliance Risk into Strategic Readiness
- 11. Further Reading
- 12. Related Articles
- Telehealth, behavioral health billing, and tribal data privacy top the list of emerging threats
- Compliance risk is shifting beyond policy into operations, staffing, and vendor oversight
- Leaders must move from reactive checklists to proactive, system-wide compliance strategies
What Is Compliance Risk in Healthcare?
Compliance risk in healthcare refers to the possibility that an organization may violate laws, regulations, or internal policies (whether intentionally or unintentionally) resulting in financial penalties, legal exposure, or reputational harm. In practical terms, this risk often shows up in areas like inaccurate billing, failure to protect patient data, improper documentation, or insufficient staff credentialing.
Every healthcare organization, regardless of size or specialty, carries compliance risk. That includes tribal health centers balancing federal oversight with sovereign governance, behavioral health facilities navigating complex payer requirements, and ambulatory groups adapting to fast-changing regulations.
A Working Definition with Operational Impact
According to the HHS Office of Inspector General (OIG), an effective compliance program includes oversight of billing practices, privacy protocols, employee training, incident response, and regular auditing. These aren’t just box-checking tasks; they’re foundational controls that keep organizations aligned with regulatory expectations and ethical care standards.
But in today’s environment, staying compliant requires more than maintaining the basics. The nature of compliance risk is shifting, and fast.
At John Lynch & Associates, we conducted a comprehensive community and document gap analysis for a behavioral health outpatient group in the Metro Phoenix area.
Through our analysis, we identified a critical gap in culturally responsive trauma-informed care, particularly for underserved adult populations experiencing co-occurring disorders.
Our findings revealed that while general therapy services were offered, the program lacked structured pathways for integrated behavioral and substance use treatment. In response, we worked closely with clinic leadership to revise the program model, incorporating evidence-based dual-diagnosis services and expanding partnerships with local recovery resources.
This shift not only aligned the clinic’s scope with pressing community needs but also positioned them for enhanced reimbursement opportunities and long-term sustainability under AHCCCS guidelines.
Why Compliance Risk Is Evolving
Several converging forces are changing the shape and scale of risk across the industry:
- Expanded use of telehealth and virtual care, creating new coding and documentation challenges
- Heightened scrutiny around behavioral health billing and credentialing
- Increased regulatory activity related to data privacy, AI integration, and cross-system interoperability
- Staffing shortages that expose compliance vulnerabilities through missed documentation or errors
What used to be a stable checklist of rules is now a dynamic, high-stakes environment where leaders must anticipate risk before it becomes a crisis.
Risk #1 – Telehealth Fraud and Reimbursement Pitfalls
The Expansion of Virtual Care Has Outpaced Oversight
The rapid growth of telehealth has unlocked critical access for patients, especially in rural and underserved communities. But it’s also exposed significant gaps in how care is documented, coded, and reimbursed. Many healthcare organizations expanded their virtual services during the pandemic without fully aligning their workflows to updated payer and regulatory requirements.
Now, as CMS and commercial payers catch up, we’re seeing increased audit activity and post-payment reviews focused on telehealth encounters; particularly in behavioral health and ambulatory care settings.
Where Compliance Risk Lives in Telehealth
Common telehealth compliance risks include:
- Missing or inconsistent documentation of time, modality (audio vs. video), and patient consent
- Billing for services that lack medical necessity under virtual conditions
- Using incorrect place-of-service or modifier codes
- Incomplete credentialing or supervision protocols for virtual providers
These may sound like technical issues, but collectively they pose a serious compliance risk—particularly when multiplied across hundreds or thousands of claims.
What Healthcare Leaders Should Do Now
To reduce telehealth compliance risk, organizations should:
- Audit a random sample of telehealth encounters monthly, reviewing documentation, coding, and consent forms
- Train clinical and billing staff on the latest payer-specific telehealth policies, including modifier usage and state-by-state rules
- Ensure that telehealth workflows mirror in-person standards, especially for intake, progress notes, and time tracking
- Consider technology updates that automatically capture modality and timestamps within your EHR
The challenge with telehealth compliance isn’t just staying current—it’s building repeatable systems that keep your organization aligned as policies continue to evolve.
Risk #2 – Behavioral Health Billing and Credentialing Gaps
Complexity Is the Norm in Behavioral Health
Behavioral health organizations face one of the most complicated reimbursement landscapes in healthcare. Unlike standard medical practices, Behavioral health providers often bill for a blend of services: therapy, medication management, group interventions, and case management—across multiple payers and care settings. Add in a variety of provider types (psychiatrists, LCSWs, peer support specialists, etc.), and compliance risk increases exponentially.
These complexities often lead to unintentional billing errors, credentialing mismatches, and supervision gaps that trigger audits or payment denials. What’s more, behavioral health is currently under increased regulatory scrutiny as payers and regulators work to enforce mental health parity and ensure proper use of public funds.
Where Risk Shows Up in Daily Operations
Some of the most common compliance gaps we see in behavioral health include:
- Billing under incorrect or expired provider credentials
- Services rendered by staff who aren’t properly licensed or supervised according to payer guidelines
- Failure to update payer rosters or maintain credentialing documentation
- Inaccurate or incomplete documentation to support medical necessity
- Misuse of time-based CPT codes, particularly for therapy sessions
These issues often stem not from neglect, but from a lack of integration between HR, credentialing, and billing systems; especially in growing organizations where new staff are added rapidly.
Strategies to Reduce Behavioral Health Compliance Risk
Leaders in behavioral health should focus on building systems that ensure accuracy and accountability across teams:
- Implement an automated credentialing tracking system that alerts teams to expirations and recredentialing needs
- Establish workflows that verify license type and supervision status before billing occurs
- Review payer contracts regularly to ensure up-to-date awareness of specific billing requirements
- Conduct focused documentation audits for therapy and group services on a quarterly basis
- Ensure billing teams are trained to correctly apply CPT codes based on session length and modality
Reducing compliance risk in behavioral health starts with recognizing operational blind spots. By tightening coordination between clinical, HR, and billing departments, organizations can move from reactive problem-solving to proactive risk management.

Risk #3 – Tribal Healthcare Data Privacy Pressures
A Complex Intersection of Regulations and Sovereignty
For tribal healthcare organizations, data privacy isn’t governed by a single standard. Instead, it sits at the intersection of HIPAA, 42 CFR Part 2, tribal sovereignty, and emerging technologies like AI and cloud-based EHRs. Each of these frameworks brings its own obligations and restrictions, often overlapping, and at times conflicting.
Unlike most healthcare organizations, tribal health programs must consider not just compliance with federal rules, but also how data governance decisions align with their community’s rights, values, and autonomy.
Hidden Risks in Health IT Infrastructure
As more tribal health organizations adopt interoperable systems or partner with outside vendors, new privacy risks emerge. Some of the most pressing include:
- Unclear data ownership when records are stored in third-party platforms
- Unauthorized access due to broad user permissions across multiple systems
- Noncompliance with 42 CFR Part 2, especially in behavioral health documentation
- Insufficient staff training on privacy policies tailored to tribal protocols
- Lack of tribal-specific policies guiding data sharing or breach response
These risks can create tension between the need for care coordination and the imperative to protect patient confidentiality within a sovereign context.
Strengthening Privacy Through Culturally Informed Governance
To reduce privacy-related compliance risks, tribal healthcare leaders should prioritize:
- Formalizing tribal data governance policies that clearly define ownership, access, and accountability
- Creating hybrid compliance frameworks that align HIPAA, 42 CFR Part 2, and tribal laws
- Vetting all third-party vendors for privacy, security, and jurisdictional awareness
- Involving tribal councils and elders in setting privacy standards and breach protocols
- Providing ongoing staff training that includes both regulatory and cultural perspectives
The goal isn’t just to avoid violations; it’s to build a privacy environment that respects both the letter of federal law and the spirit of tribal sovereignty.
Risk #4 – Inadequate Incident Response and Breach Readiness
Compliance Is Also About Recovery
When most healthcare leaders think about compliance, they focus on prevention (policies, training, audits). But compliance risk doesn’t end once something goes wrong. In fact, how an organization responds to an incident is increasingly a factor in enforcement actions and financial penalties.
The Office for Civil Rights (OCR) and other regulators now assess not only whether a breach occurred, but whether the organization had a tested and timely response in place. For healthcare organizations, especially those dealing with sensitive data like behavioral health or tribal records, being unprepared to respond can amplify legal and reputational damage.
Common Gaps in Incident Response Planning
In our consulting work, we frequently encounter incident response plans that are:
- Outdated or missing entirely
- Generic templates not tailored to the organization’s structure or systems
- Unknown to key staff, especially those outside IT or compliance
- Missing clear guidance on roles, communication, or patient notification
Even organizations with strong preventive controls can fall short when an event occurs, particularly if teams don’t know how to escalate, who to contact, or what protocols to follow.
How to Build an Effective Breach Response Plan
To improve breach readiness, healthcare leaders should ensure that their response plan includes:
- A designated incident response team with defined roles across clinical, IT, legal, and communications functions
- Clear escalation protocols for reporting suspicious activity, unauthorized access, or potential breaches
- Templates and timelines for patient notification, regulatory reporting, and media response
- Regular tabletop exercises to test the plan under real-world scenarios
- Post-incident review procedures that lead to system and policy improvements
An effective response doesn’t just limit liability; it also builds trust with patients, staff, and regulators. It sends the message that compliance isn’t just a checkbox; it’s embedded in the organization’s culture and operations.

Risk #5 – Third-Party Vendor Oversight and Contract Compliance
The Compliance Risks You Don’t See Coming
Healthcare organizations increasingly rely on third-party vendors for everything from EHR hosting to revenue cycle management. While these partnerships bring efficiency and scale, they also introduce significant compliance risk; especially when oversight is limited to contract signing.
Too often, vendor-related breaches or violations catch leaders by surprise, only to reveal gaps in monitoring, unclear contract language, or missing safeguards altogether. And because the organization (not the vendor) is ultimately responsible for patient data and regulatory compliance, the consequences can be costly.
Where Vendor Compliance Risk Lives
Common risk areas tied to third-party vendors include:
- Incomplete or outdated Business Associate Agreements (BAAs)
- Weak data security practices by vendors handling protected health information (PHI)
- Lack of audit or breach notification rights written into contracts
- Poor alignment with HIPAA, 42 CFR Part 2, or tribal data governance policies
- Minimal or no regular performance reviews or compliance checks
These gaps can expose your organization to OCR penalties, contract disputes, or operational disruption if a vendor fails to meet compliance expectations.
Strengthening Third-Party Oversight
To reduce vendor-related compliance risk, healthcare leaders should build stronger internal governance around procurement, contracting, and vendor management. This includes:
- Maintaining a centralized vendor inventory with risk ratings and contract expiration dates
- Ensuring all BAAs and service contracts include clear audit rights, data protection clauses, and breach reporting timelines
- Requiring vendors to demonstrate security and compliance certifications (e.g., SOC 2, HITRUST) during procurement
- Conducting annual vendor risk assessments and documenting findings
- Involving compliance and IT teams in contract negotiations and vendor performance reviews
Managing third-party risk is an ongoing responsibility, not a one-time decision. By integrating compliance considerations into vendor relationships from the start, and maintaining consistent oversight, healthcare organizations can reduce exposure and maintain trust across every level of their operations.
Risk #6 – Staffing Shortages Leading to Operational Gaps
Burnout and Short Staffing Increase Compliance Exposure
Workforce challenges are affecting nearly every corner of healthcare, from front desk staff to credentialed providers and coders. While the clinical impact of staffing shortages is well known, compliance risks are often underestimated.
When staff are stretched thin, rushed, or unfamiliar with updated protocols, mistakes happen. Documentation shortcuts, missed deadlines, and inconsistent processes all open the door to violations. Worse, when these issues are systemic, they can signal noncompliance even if there was no intent to deceive or defraud.
Where Gaps Are Most Common
Some of the most vulnerable points in under-resourced environments include:
- Intake and eligibility verification: Errors here can lead to improper billing or delayed reimbursement
- Clinical documentation: Rushed or missing notes compromise medical necessity and coding accuracy
- Coding and billing: Backlogs and misassignments increase denial risk and trigger audits
- Credentialing: Delays in onboarding or tracking renewals can result in noncompliant service delivery
Many of these issues stem from a combination of burnout, turnover, and limited cross-training; factors that are all within leadership’s ability to address.
Proactive Responses to Staffing-Driven Compliance Risk
Rather than waiting for a compliance failure to reveal operational cracks, organizations can take steps to build resilience across teams:
- Conduct a compliance-focused workflow audit to identify where tasks are being dropped or delayed
- Invest in targeted micro-trainings for high-risk roles, such as intake coordinators and coders
- Use technology to streamline repetitive documentation or automate simple verifications
- Build redundancy into critical roles, ensuring compliance doesn’t rest with one overburdened employee
- Make compliance a shared responsibility, not just a departmental silo
When staffing is tight, organizations must work smarter to protect against risk. By recognizing the link between workforce health and compliance integrity, leaders can close the gap before it becomes a liability.

Risk #7 – Rapid Changes in Healthcare Regulations
The Rulebook Keeps Changing
Over the past few years, regulatory updates in healthcare have accelerated, not only in volume, but also in complexity. From new rules around price transparency and interoperability to updates in mental health parity enforcement, AI oversight, and data sharing, the compliance landscape is becoming harder to navigate.
These changes affect all healthcare organizations, but those with limited internal policy tracking or cross-departmental communication are most at risk. When rules change faster than internal processes can adapt, compliance failures are often the result.
Trends to Watch in 2025 and Beyond
Several regulatory trends are shaping the risk environment for healthcare leaders:
- Behavioral health parity enforcement: Increased audits to ensure coverage and reimbursement equity with physical health
- AI use in clinical settings: New scrutiny over bias, explainability, and compliance with informed consent standards
- Patient data portability: Greater requirements for timely access to records under the 21st Century Cures Act
- CMS reimbursement model changes: Continued evolution of value-based care metrics and quality reporting
- Price transparency expansion: Tighter rules around disclosure of costs and coverage estimates
These evolving areas require more than compliance awareness; they demand operational alignment across departments.
Assigning Ownership and Creating Responsiveness
To stay ready for regulatory change, organizations should:
- Designate a compliance lead or task force responsible for monitoring federal and state updates
- Create quarterly cross-functional reviews to assess policy impacts and action plans
- Maintain version-controlled policies and procedures that reflect current standards
- Subscribe to trusted industry sources and legal alerts to catch changes early
- Conduct annual policy refreshes tied to strategic planning
Regulatory changes don’t always come with long lead times. The most compliant organizations aren’t just rule-followers; they’re agile systems that can adjust as the environment shifts.
Building a Future-Ready Compliance Strategy
From Reactive Compliance to Operational Resilience
Healthcare organizations that treat compliance as an afterthought, or worse, a one-time project, leave themselves exposed. The reality is that compliance risk isn’t going away, and it won’t get simpler. The organizations that will thrive in the next era of healthcare are those that bake compliance into every part of their operation: workforce development, vendor relationships, billing workflows, and strategic planning.
Compliance is no longer just about checking boxes. It’s about building resilient systems that align with your mission, support your staff, and meet evolving regulatory expectations.
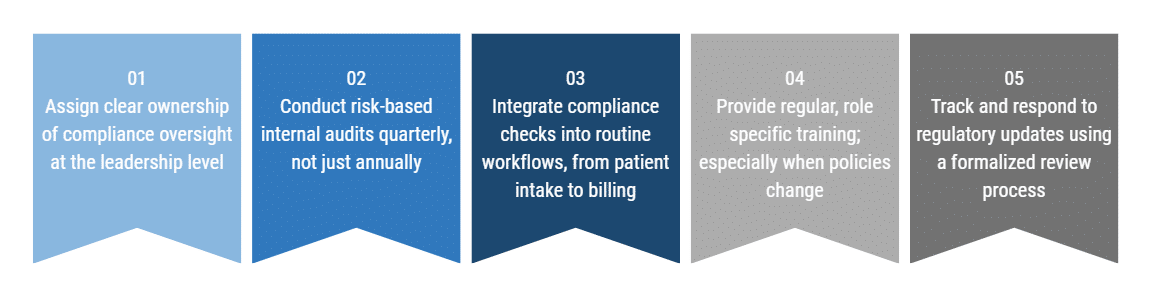
5 Ways to Strengthen Compliance from the Inside Out
To make compliance a living part of your organization, consider these steps:
By treating compliance as a continuous improvement process, leaders can shift from reacting to problems to building proactive, audit-ready cultures.
A Tool to Help You Start
To help your team assess current strengths and vulnerabilities, we’ve created a practical resource:
Download our Healthcare Compliance Review Checklist
This free tool walks through key compliance categories. From documentation and credentialing to vendor management, it can serve as the foundation for your next internal review or planning session.
Turning Compliance Risk into Strategic Readiness
A Time of Growing Scrutiny and Opportunity
Compliance risk in healthcare demands active leadership, thoughtful planning, and organization-wide accountability. As regulatory demands grow more complex and interconnected, healthcare organizations that respond with clarity, agility, and foresight will be better positioned to serve their communities and protect their operations.
What once felt like a behind-the-scenes function must now be treated as a central pillar of organizational strategy.
The Path Forward
Whether you’re managing a tribal health system, behavioral health facility, or ambulatory care network, the message is the same: compliance must evolve with your organization. That means moving beyond reactive audits and toward embedded, proactive systems that reduce risk and support long-term success.
By aligning compliance with your mission and operations, you’re not just avoiding penalties, you’re creating a stronger, more resilient foundation for care.
Ready to Talk?
Further Reading
John Lynch & Associates
- Healthcare Compliance Review Checklist
A practical tool to help assess compliance strengths and vulnerabilities across key operational areas.
U.S. Department of Health & Human Services (OIG)
-
Compliance Guidance
Official guidance on developing and maintaining effective healthcare compliance programs.