Electronic Health Records (EHRs) are often seen as tools for documentation, compliance, and billing. In Tribal health systems, they represent something far more critical: a gateway to care.
When EHR systems are not designed or optimized with the realities of Tribal communities in mind, they can unintentionally create delays, confusion, and barriers that prevent patients from getting the care they need, when they need it.
From missed appointments due to clunky scheduling portals to limited access to medical histories across departments, underperforming EHRs affect more than just efficiency; they affect lives.
In an environment where health disparities persist and access to culturally competent care remains uneven, every missed connection through an EHR system widens the gap.
For Tribal leaders and health administrators, now is the time to ask: Is our EHR system helping patients access care, or making it harder?
This article explores how EHR design and usability influence patient access in Tribal health systems, why this is a mid-year priority, and how leaders can reframe EHR optimization as a meaningful path toward health equity.
- 1. Article Highlights
- 2. Understanding the Landscape of Tribal Health Systems
- 3. The Role of EHRs in Improving (or Hindering) Patient Access
- 4. Hidden Barriers in Tribal EHR Systems
- 5. Mid-Year EHR Reflection: Is Your System Supporting Patient Access?
- 6. Reframing EHR as a Tool for Equity
- 7. Recommendations: Building Culturally Responsive EHR Strategies
- 8. Turning Barriers into Opportunities
- 9. Further Reading
- 10. Related Articles
Article Highlights
- Mid-year is a key opportunity for Tribal health leaders to assess EHR usability and realign systems with community needs.
- EHR systems directly impact patient access and when misaligned, they can silently widen care gaps in Tribal communities.
- Improving patient access through EHRs requires culturally responsive design, training, and strategies that prioritize whole-person care.
Understanding the Landscape of Tribal Health Systems
To fully grasp the impact of EHR systems on patient access in Tribal communities, it's essential to understand the broader context in which these systems operate. Tribal health systems are uniquely shaped by a long history of underfunding, federal oversight, and the sovereign right of Tribal Nations to govern their own healthcare.
Many clinics and health centers operate within complex frameworks involving the Indian Health Service (IHS), 638 contracts, and other hybrid models that blend traditional healing with Western medicine.
These systems are often tasked with serving wide geographic areas, managing high patient-to-provider ratios, and addressing the effects of intergenerational trauma and chronic disease—often with fewer resources than their non-Tribal counterparts. In this environment, tools like EHRs must do more than function; they must empower.
Unfortunately, many off-the-shelf EHR platforms fall short. They’re not built with the cultural practices, language diversity, or interdisciplinary care models found in Tribal health settings.
The result?
Systems that may technically "work" but don't serve the full scope of the community’s needs, making it harder (not easier) for patients to navigate care.
As more Tribal leaders take steps toward self-determination in healthcare delivery, the effectiveness of EHR systems has become a reflection of something much larger: the ability of a community to shape its own pathways to health and healing.

The Role of EHRs in Improving (or Hindering) Patient Access
At their best, Electronic Health Records (EHRs) serve as a bridge between patients and providers; streamlining care coordination, improving communication, and ensuring timely access to critical health information.
In Tribal health systems, where providers often wear many hats and patients may receive care across departments like behavioral health, dental, and primary care, the promise of EHRs is especially compelling.
A well-implemented EHR system can:
- Reduce wait times through efficient scheduling,
- Enable providers to quickly access a patient’s full health history,
- Support real-time referrals across services,
- And empower patients with easier access to their own records and care plans.
But when these systems are poorly configured or lack cultural and operational alignment, that promise breaks down.
Patients may struggle with portals that aren’t mobile-friendly or available in their preferred language. Staff may work around documentation limitations, leading to incomplete records.
Siloed modules may hinder referrals and cross-department communication. In some cases, basic functions, like scheduling an appointment or viewing lab results, become points of frustration that delay care.
In Tribal communities, where trust in systems has been historically hard-won, these breakdowns aren’t just technical; they’re personal. Every missed message or disconnected workflow can lead to disengagement, missed opportunities for early intervention, or worsening chronic conditions.
What begins as a software problem quickly becomes a patient access issue and a health equity issue.
This is why Tribal health leaders must view their EHR systems not just as administrative tools, but as foundational to the delivery of equitable, coordinated care.
Hidden Barriers in Tribal EHR Systems
What are the barriers to adoption of electronic health records?
While most healthcare systems face challenges in adopting EHRs, Tribal communities encounter a unique (and often more complex) set of barriers. Many standard EHR platforms are designed for urban or private healthcare settings, leaving Tribal health programs to retrofit systems that were never intended to meet their needs.
Common barriers include:
- Cultural misalignment: Most EHRs aren’t built to reflect cultural considerations, traditional healing practices, or even language preferences. This can make documentation feel disconnected from the way care is delivered.
- Customization limitations: Many systems lack flexibility, making it difficult to track services specific to Tribal health programs, such as community health outreach, integrated behavioral health, or ceremonial care support.
- Vendor mismatches: Off-the-shelf EHRs may not account for IHS-specific reporting or 638 funding models, creating compliance headaches and limiting long-term sustainability.
What are the barriers to Native American healthcare?
Beyond technology, there are systemic obstacles that affect how care is accessed and delivered across Indian Country; many of which compound the effects of an underperforming EHR.
These include:
- Limited broadband and IT infrastructure: In rural and remote areas, internet access can be inconsistent, making EHRs difficult to use in real time.
- Staffing shortages and high turnover: Understaffed clinics often have little time for EHR training or system improvement efforts.
- Digital literacy gaps: Patients and some staff may be unfamiliar with EHR portals or digital health tools, leading to underuse and miscommunication.
- Historical mistrust in healthcare systems: Systemic barriers, when paired with non-intuitive or impersonal EHR experiences, can discourage engagement and undermine relationships with care providers.
These layers of barriers - technical, cultural, and systemic - turn what should be a tool for connection into another hurdle for both providers and patients. A study published in JAMA Health Forum found that while patient access to electronic health information has improved over time, significant racial and ethnic disparities persist, emphasizing the need for more equitable EHR implementations.
Mid-Year EHR Reflection: Is Your System Supporting Patient Access?
As we move through the second quarter of the year, now is a natural point for Tribal health leaders to pause and reflect:
Is our EHR system truly supporting patient access, or silently creating barriers?
A mid-year evaluation can help uncover misalignments between how care is delivered and how it’s documented, accessed, and coordinated through your EHR. These gaps often go unnoticed in day-to-day operations but can have a profound effect on both patient outcomes and staff efficiency.
Mid-Year EHR Self-Assessment Checklist
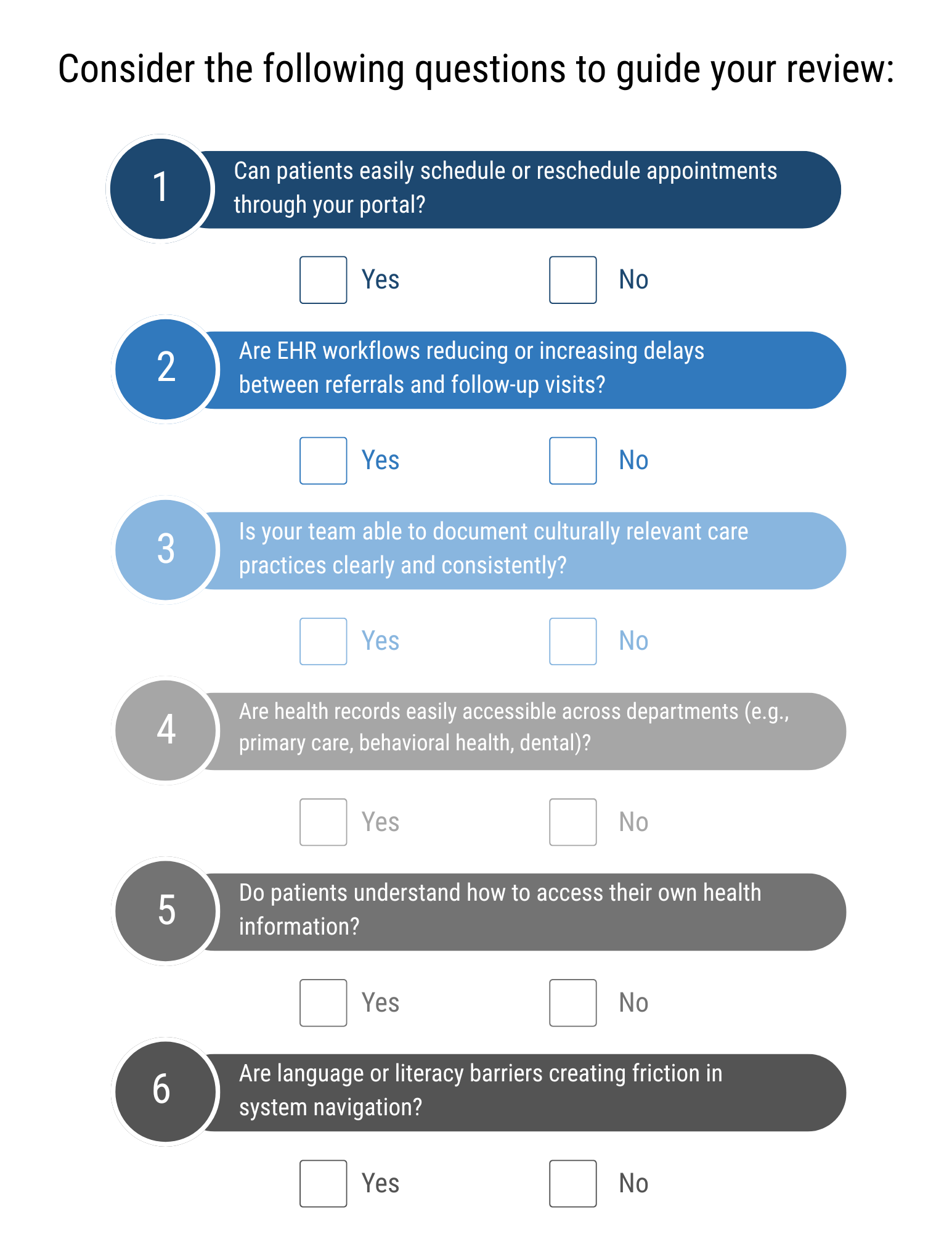
This kind of mid-year check-in not only ensures your system is aligned with care delivery goals—it creates space for proactive improvements rather than reactive workarounds.
Whether you’re planning minor adjustments or a deeper EHR optimization initiative, now is the time to reassess system performance with a focus on access, equity, and cultural alignment. John Lynch & Associates partners with Tribal health systems to guide these reviews and translate findings into strategic, community-centered improvements.
The Overlooked Link Between EHR and Revenue Cycle Health
When Tribal health leaders think about revenue cycle management (RCM), they often focus on claims, coding, and reimbursement. But what’s often overlooked is how deeply tied RCM performance is to the patient access experience, and by extension, to how well your EHR system supports it.
Here’s how underperforming EHRs can silently undermine your revenue cycle:
Access Issues That Lead to Revenue Loss
- Missed appointments: When patients struggle to navigate a confusing portal or receive no confirmation of scheduled visits, no-shows increase, and with them, revenue loss.
- Delayed care and documentation gaps: If your EHR doesn’t support quick referral tracking or timely documentation, care gets delayed, and claims are often incomplete or denied.
- Data inaccuracies: Poor usability can lead to inconsistent demographic, insurance, or clinical data, resulting in denied or delayed claims.
- Overburdened staff: When providers or billing teams are bogged down by inefficient workflows, they’re less able to focus on accuracy and timeliness - two pillars of healthy RCM.
In a setting where every dollar is stretched to meet broad community needs, these issues compound quickly. Investing in EHR usability isn’t just about patient experience; it’s about financial sustainability.
A mid-year review of your EHR’s impact on both patient access and billing workflows can help uncover low-effort improvements with high return - both in patient satisfaction and operational health.
To take that review further, Tribal health leaders should evaluate their financial performance against key revenue cycle metrics. This RCM performance benchmarks guide outlines critical indicators that can reveal where EHR workflow breakdowns are silently costing your organization time and revenue.
Reframing EHR as a Tool for Equity
How does EHR improve patient access to care?
Despite the challenges, EHR systems hold real potential to promote health equity in Tribal communities - if they are thoughtfully implemented and aligned with how care is delivered and received.
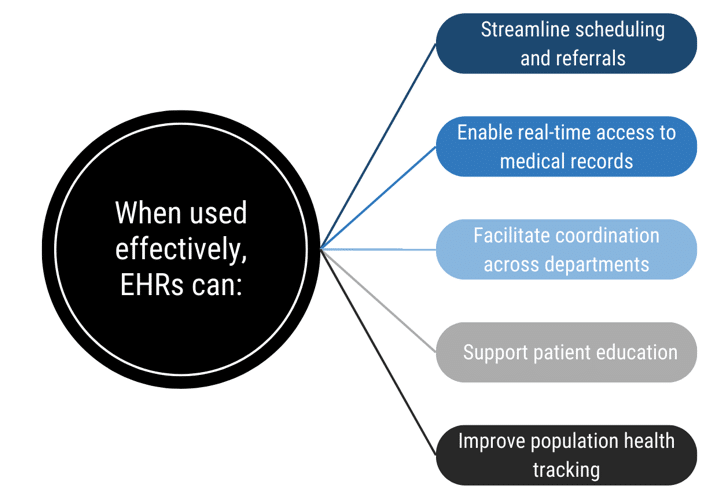
When used effectively, EHRs can:
- Streamline scheduling and referrals, reducing wait times and improving continuity of care.
- Enable real-time access to medical records, empowering both providers and patients to make informed decisions.
- Facilitate coordination across departments, including behavioral health, dental, and chronic disease management, which is vital in whole-person care.
- Support patient education by making care plans, medication instructions, and follow-up tasks more transparent and accessible.
- Improve population health tracking, allowing leadership to identify trends, allocate resources, and measure progress toward community health goals.
But none of these benefits are automatic. They depend on systems that are usable, accessible, and culturally responsive.
For EHRs to support equity, they must go beyond data capture. They must remove friction from the care experience, support provider-patient trust, and adapt to the unique needs of Native communities. The adoption and meaningful use of EHR technology can help reduce health disparities among American Indian and Alaska Native populations by providing reliable, consistent patient data that follows patients wherever they receive care.
This shift begins when Tribal health leaders view EHR optimization not as an IT project, but as a core strategy for improving access, deepening community engagement, and advancing long-term health outcomes.
Recommendations: Building Culturally Responsive EHR Strategies
Improving patient access through EHR systems requires more than just upgrades—it calls for a fundamental shift in how systems are designed, selected, and supported. For Tribal communities, that means EHRs must reflect local values, respect cultural practices, and be flexible enough to serve diverse care delivery models.
Here are key recommendations for Tribal health leaders looking to move their EHRs from obstacles to equity tools:
- Engage Community Voices from the Start: Involve Tribal leaders, frontline staff, and community members in the assessment and decision-making process. Their lived experience is essential to shaping workflows, interfaces, and documentation practices.
- Choose Systems That Allow for Customization: Work with EHR vendors who understand the nuances of Tribal health systems—or who are open to building them in. This includes modules for community outreach, traditional care, and multi-generational family health histories.
- Integrate Language and Cultural Relevance: Ensure the system and any patient-facing portals reflect language diversity and cultural sensitivity. Whether it's translating interface elements or including traditional wellness terms in documentation, small adjustments can build trust and improve usability.
- Invest in Targeted Training and Support: Digital literacy isn’t one-size-fits-all. Offer training tailored to various roles—from CHRs to medical assistants to community members—and keep resources accessible long after go-live.
- Design for Interoperability and Whole-Person Care: Make sure the EHR supports seamless communication across departments, enabling coordinated care for behavioral, dental, and primary health—all of which may be provided in a single visit.
These aren’t just best practices—they’re prerequisites for systems that truly serve Tribal communities. And they reflect a deeper truth: when technology is shaped by the community it’s meant to serve, it becomes a tool for sovereignty, self-determination, and long-term health equity.
Turning Barriers into Opportunities
Electronic Health Records should be a bridge—not a barrier—between patients and the care they need. Yet for many Tribal health systems, misaligned EHRs are silently contributing to missed appointments, delayed care, and growing gaps in equity.
This is not just a technology problem—it’s a care access issue. And mid-year is the ideal time for Tribal health leaders to step back and ask: Is our EHR helping us deliver the care our community deserves?
The good news? With the right support, EHRs can be transformed into powerful tools that promote connection, streamline access, and reinforce culturally grounded care. It starts with acknowledging the hidden challenges—and committing to systems built around the lived realities of Tribal communities.
At John Lynch & Associates, we partner with Tribal health leaders to assess, optimize, and realign EHR systems that support whole-person care, patient engagement, and operational strength. Whether you’re facing usability challenges, access issues, or revenue impacts, we’re here to help you turn technology into a true asset for your community.
Ready to Talk?
Further Reading
Explore additional insights and tools to support stronger EHR systems, improved patient access, and health equity in Tribal health:
- Top EHR Implementation Challenges and How to Overcome Them
Uncover common barriers in EHR rollouts—and how Tribal health systems can overcome them with tailored strategies.
- RCM Performance Benchmarks and Metrics Guide
Use key performance indicators to identify how EHR and workflow issues may be impacting revenue and access.
- Mastering IHS Standards: Ensuring Compliance & Quality Care
Align your EHR and operational systems with IHS standards to support both compliance and culturally grounded care delivery.
- Progress and Persistent Disparities in Patient Access to Electronic Health Information – JAMA Health Forum
This study highlights ongoing disparities in electronic health information access, reinforcing the importance of inclusive EHR design.
- Health IT-Enabled Infrastructure for Reducing AI/AN Health Disparities – HealthIT.gov
Explores how health IT can support equitable care delivery for American Indian and Alaska Native populations through better data access.
Related Articles

Reducing Risk in Tribal Health with Staff Compliance Training

A Comprehensive Tribal Health IT Strategy for Modern Tribal Health Leaders