For behavioral health leaders preparing to open a new clinic, May often feels like the final sprint. The vision is clear. The funding is in place. The target go-live date is just around the corner. But as the opening draws near, operational cracks that were manageable earlier in the process begin to widen.
This is the moment when “almost ready” becomes a dangerous place to be.
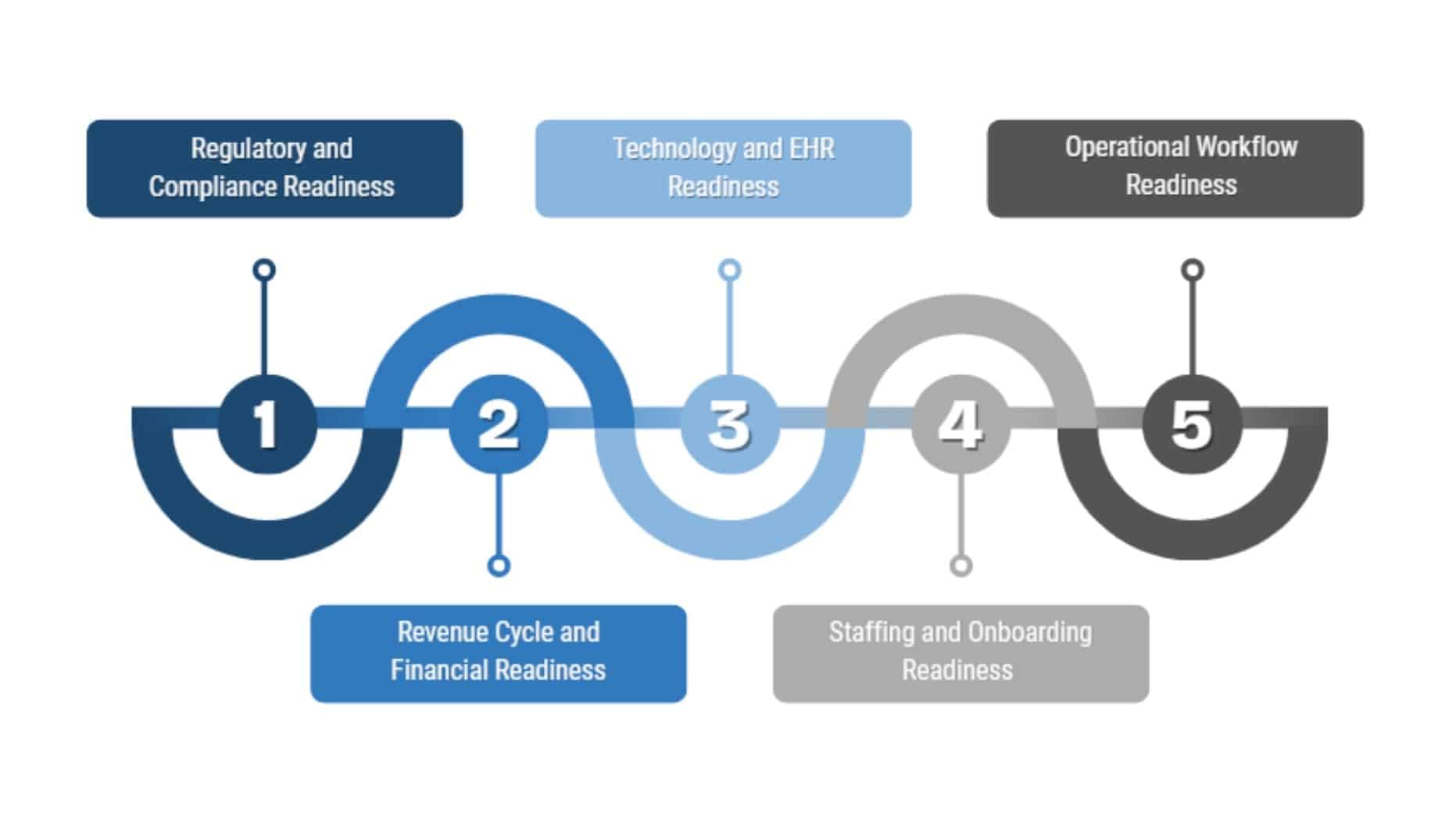
- 1. Why “Almost Ready” Isn’t Ready Enough
- 2. The 5 Most Common Last-Minute Pitfalls in Behavioral Health Expansion
- 3. A Smarter Path to Behavioral Health Clinic Startup Readiness
- 4. Final Readiness Checklist for Behavioral Health Clinic Leaders
- 5. You’re Not Alone in the Final Stretch
- 6. Further Reading
- 7. Related Articles
- Regulatory delays and missing licensure steps can stall your opening early planning is essential.
- Revenue cycle and EHR misalignment create downstream financial and operational risks.
- Workflow testing, onboarding, and cross-functional planning turn chaos into confident care delivery.
Why “Almost Ready” Isn’t Ready Enough
Launching a behavioral health clinic is more than turning on the lights and scheduling appointments. It requires synchronized planning across licensing, revenue cycle management, staffing, EHR configuration, and workflow execution.
If just one of those areas is underdeveloped or overlooked, the ripple effect can delay opening day, disrupt care delivery, or lead to costly compliance failures.
What many leaders discover in the final stretch is that seemingly small oversights carry big consequences. Missing a single licensure step can stall your ability to bill payers. Inadequate staff onboarding can lead to errors, low morale, and turnover.
Unresolved EHR configuration issues can clog documentation workflows and frustrate clinicians. At a time when patient demand is surging, these breakdowns can feel like failure.
But they aren’t failures. They’re signs that the process needs structure, support, and a final readiness check.
In this article, we’ll walk through five of the most common last-minute pitfalls organizations face during a behavioral health clinic startup. We’ll also share insights on how to avoid them through strategic planning, cross-functional coordination, and the right partnerships.
Let’s make sure your clinic is not just “almost ready” but fully prepared to launch with confidence.
The 5 Most Common Last-Minute Pitfalls in Behavioral Health Expansion
#1. Regulatory Gaps and Licensing Delays
Each state outlines its own behavioral health licensing requirements, and those requirements can vary not just by location, but by level of care and service type. Even small missteps in documentation or timing can derail a clinic's ability to open or bill.
While licensing itself is handled at the state level, it exists within a broader policy environment shaped by federal regulations. The Substance Abuse and Mental Health Services Administration provides an overview of national laws and regulatory policies that guide behavioral health service delivery and compliance expectations.
Leaders often underestimate how long it takes to complete credentialing, navigate inspections, or respond to agency feedback. Others assume they can begin care delivery while paperwork is still processing, not realizing that doing so may result in financial or legal consequences.
We’ve worked with organizations who were just weeks from opening when they realized their licensure applications were incomplete or misaligned with their service delivery model. In one case, a behavioral health clinic had built out a strong staffing plan and IT infrastructure but had not accounted for state-level requirements tied to their intensive outpatient programming.
They turned to our team for support. Within days, we helped them map out a corrective plan, coordinate directly with the regulatory agency, and resubmit the necessary documentation to avoid a costly launch delay.
These types of last-minute challenges are avoidable with the right structure in place. Leaders should begin licensing conversations early, build regulatory checkpoints into their launch timeline, and assign ownership to someone who will actively manage the process rather than treat it as a task to check off. Conducting a pre-launch compliance review that includes documentation, policies, and payer readiness helps ensure nothing critical falls through the cracks.
Regulatory readiness is not just about ticking boxes. It is about building a clinic that can open on time, serve its community without disruption, and move forward with confidence.
#2. Revenue Cycle Blind Spots
One of the most common blind spots is failing to complete payer credentialing in advance. Without approved provider enrollment, claims may be denied or delayed for weeks sometimes months. Additionally, startup teams often assume their existing billing processes can be duplicated at a new site without accounting for volume changes, payer mix differences, or gaps in documentation training. These assumptions can severely disrupt cash flow within the first 30 to 60 days of operation.
We worked with a behavioral health organization that launched a second location confident in their clinical setup, but had not completed credentialing for half of their provider team. Claims were submitted, services were delivered, but reimbursements never came.
By the time they reached out for help, the clinic was already facing financial strain. Our team quickly assessed the gaps, facilitated urgent outreach to payers, and built a corrected billing workflow that stabilized operations, but not before weeks of avoidable revenue loss.
These types of disruptions are preventable. Effective revenue cycle planning begins well before launch, with a detailed review of credentialing status, internal billing workflows, and payer-specific documentation requirements.
It also includes educating front office staff and clinicians on the key points of clean claim submission. Overlooking any part of this process can cost more than just time; it can threaten the financial sustainability of a new clinic.
If your billing plan still feels unfinished, or if you’re unsure whether your team is equipped to support a new location, it is critical to understand the financial pitfalls that often emerge when revenue cycle planning is rushed or incomplete and how to address them before they escalate.
#3. EHR and Technology Misalignment
Each new clinic has its own workflows, provider preferences, and patient population needs. If the EHR is not customized to reflect those differences, documentation backlogs, user frustration, and data capture issues can quickly follow.
This is especially true in behavioral health, where the complexity of intake, progress notes, care coordination, and reporting often exceeds the capabilities of default system templates.
We partnered with a behavioral health provider that had used the same EHR for years with moderate success. However, during their clinic expansion, they neglected to review how their existing setup would function in a higher-volume, multi-site environment.
Within days of opening, the team was overwhelmed by incomplete documentation, billing delays, and system confusion. Our consultants worked closely with clinical, administrative, and IT leaders to reconfigure workflows, provide targeted training, and establish clear documentation protocols aligned with the needs of the new site.
These issues are more common than most leaders realize. As we have seen across multiple engagements, the inefficiencies caused by misaligned EHR workflows can ripple across operations and ultimately affect patient care, revenue, and staff satisfaction.
To prevent EHR-related setbacks, organizations should conduct an early technical readiness assessment before launch. This includes reviewing user access, templates, documentation workflows, and reporting functionality specific to the services the new clinic will offer.
Investing in this step can significantly reduce downstream disruptions and improve staff confidence on day one.
#4. Staff Onboarding Bottlenecks
New behavioral health clinics typically face two onboarding challenges at once: bringing new staff into the organization and preparing them to deliver services in a newly built workflow. If those workflows are not well defined, or if training is left to “on-the-job learning,” the results can be costly.
Staff may not know how to document correctly, follow intake protocols, or navigate EHR systems. Worse, without proper orientation to the clinic’s culture and expectations, they may disengage quickly.
In one clinic expansion we supported, leadership had done an excellent job of hiring in advance but underestimated the time and coordination required for onboarding. The result was a talented staff unsure of their roles, unfamiliar with clinical workflows, and frustrated by a lack of structured support.
We stepped in to assess the gaps, develop a training timeline, and facilitate onboarding that aligned with the clinic’s opening schedule. Within two weeks, the team was aligned, confident, and moving forward together.
Strong onboarding starts with preparation. Leaders should ensure that every role has a defined scope, training plan, and access to the systems they need to succeed.
Scheduling mock workflows, shadowing opportunities, and team orientation meetings before launch helps eliminate first-day confusion. The goal is not just to fill seats, but to empower people to deliver great care from day one.
#5. Skipping Workflow Testing and Operational Dry Runs
Launching without a dry run is like putting a car on the road without checking the brakes. Intake processes, documentation flows, referral handoffs, and billing steps may all seem clear on paper, but the reality of delivering care in a live environment often reveals gaps that slow everything down.
These disruptions can lead to delayed services, staff confusion, and patient dissatisfaction; outcomes no organization wants during its critical first days.
We have supported clinics where the absence of workflow testing led to immediate setbacks. In one case, clinicians were unsure of when to complete treatment plans in the EHR, front office staff didn’t have a clear intake script, and internal handoffs created delays that stretched patient visits by over an hour.
After conducting a structured operational dry run with all departments, the team was able to identify friction points and realign processes before opening day.
Workflow testing should be treated as a core part of launch readiness, not an optional exercise. Running mock scenarios, role-playing patient visits, and reviewing documentation cycles in real time allow staff to work out the kinks before real patients are involved. This not only prevents costly inefficiencies, but it also builds team confidence and cohesion.
The more a team practices together before go-live, the more prepared they are to deliver coordinated, high-quality care when it counts most.

A Smarter Path to Behavioral Health Clinic Startup Readiness
Avoiding last-minute setbacks requires more than problem-solving at the finish line. It calls for a deliberate, integrated approach that connects every function involved in launching a behavioral health clinic. Compliance, clinical operations, finance, IT, and leadership must all move in sync.
When these areas work independently, small missteps can quickly escalate into costly delays. But when aligned early, the path to a smooth and successful launch becomes much clearer.
Build a Cross-Functional Launch Plan
Successful clinic startups begin with shared ownership. That means engaging the right people from the very beginning. Clinical leads, billing experts, compliance officers, and IT stakeholders each bring critical insight to the process.
By mapping out the launch timeline together, organizations can identify interdependencies and risks before they cause disruption. For example, will new staff be trained on workflows that have not yet been tested? Are payer credentialing deadlines coordinated with projected go-live dates? Are EHR templates ready for the appropriate level of care?
Too often, these questions surface only after problems emerge. Holding a cross-functional planning session early in the project helps ensure that all teams are aligned. It also builds a culture of shared responsibility, which becomes essential during the unpredictable days leading up to launch.
Leverage Strategic Partners to Fill Gaps
Even the most capable teams can run short on time or capacity during a clinic expansion. In these moments, external support becomes more than helpful. It becomes essential. Strategic partners bring fresh perspective, deep expertise, and the ability to manage complex tasks without pulling internal staff away from their core responsibilities.
In one expansion project, our team at John Lynch & Associates was brought in to support a clinic that had lost momentum midway through its launch. The internal team was stretched thin, and several critical areas including EHR configuration and regulatory documentation had fallen behind.
We provided interim leadership, facilitated a rapid recovery plan, and worked alongside staff to bring everything into alignment. The clinic opened just two weeks later than planned, avoiding a projected two-month delay.
In situations like these, interim healthcare leadership can be the difference between recovery and derailment. Whether support is needed in project management, compliance, or system readiness, having experienced partners in place ensures that nothing gets missed when it matters most.
Final Readiness Checklist for Behavioral Health Clinic Leaders
Before opening day, every behavioral health clinic startup should pause to ask one essential question: are we truly ready to deliver care, operate efficiently, and remain compliant on day one?
A readiness checklist brings clarity to that question. It translates big-picture planning into actionable steps, making it easier to confirm what is complete, what is in progress, and what still needs attention. Whether your launch is two months away or two weeks out, walking through this list with your leadership team can help prevent last-minute surprises.
Regulatory and Compliance Readiness
- All state licensure requirements are submitted, tracked, and approved
- Accreditation or inspection timelines are confirmed
- Required documentation and policies are finalized and accessible
- Payer enrollment is complete and verified
Revenue Cycle and Financial Readiness
- Billing workflows are tested and aligned with services offered
- Payer credentialing is complete for all providers
- Staff understand documentation and coding requirements
- Financial forecasting accounts for startup phase cash flow
Technology and EHR Readiness
- EHR templates match the clinical model and service lines
- User access and permissions are properly configured
- Reporting tools are functional and validated
- Staff have received training on documentation workflows
Staffing and Onboarding Readiness
- All roles are filled or covered by interim support
- Onboarding plans are developed and in progress
- Staff understand their roles, workflows, and escalation paths
- Team culture and expectations have been clearly communicated
Operational Workflow Readiness
- Intake, treatment planning, and discharge workflows are mapped and tested
- Dry runs or mock clinics have been completed
- Internal handoffs and documentation steps are rehearsed
- Leadership has a communication plan for go-live week
You’re Not Alone in the Final Stretch
Opening a new behavioral health clinic is a bold and meaningful step toward expanding access to care. But in the final weeks before launch, even the most prepared teams can feel overwhelmed.
It is common to second-guess decisions, discover missing pieces, or simply run out of time. These are not signs of failure. They are signs that support may be needed to finish strong.
No one should have to navigate this critical phase alone. Whether the challenge is regulatory, operational, technical, or financial, there is always a path forward with the right structure and the right people beside you. John Lynch & Associates partners with behavioral health leaders to turn last-minute risks into coordinated, confident action.
With deep experience in clinic startups and expansion efforts, we help you launch not only on schedule, but with systems and strategies that are built to sustain growth.
Ready to Talk?
Further Reading
- Substance Abuse and Mental Health Services Administration (SAMHSA)
Laws, Regulations, and Policies
An overview of the federal laws and regulatory frameworks that guide behavioral health service delivery and influence state-level compliance expectations. John Lynch & Associates.
Behavioral Health Billing: Tips to Overcoming Challenges
Key insights into common billing pain points and how to prepare financially before launching or expanding services. - John Lynch & Associates
The Hidden Cost of EHR Workflow Inefficiency in Behavioral Health
How poorly configured EHR systems impact care delivery, documentation, and operational efficiency in behavioral health settings. - John Lynch & Associates
Navigating CIO Vacancies with Interim Leadership
A look at how interim healthcare leaders can step in during times of transition to stabilize complex projects like clinic expansion or system implementation.
Related Articles

Audit Readiness in Behavioral Health: How Compliance Officers Lead Beyond the Checklist

3 Strategies to Improve Behavioral Health Financial Stability