- 1. What Is Healthcare Performance Improvement?
- 2. How to Improve Health System Performance
- 3. What Are Examples of Performance Improvement in Healthcare?
- 4. Why Time Management in Healthcare Drives Efficiency
- 5. A Practical Framework for Healthcare Process Improvement
- 6. Conclusion: Efficiency Is a Strategy, Not Just a Goal
- 7. Further Reading
- 8. Related Articles
- Healthcare performance improvement focuses on better care delivery, workflow optimization, patient outcomes, and cost control.
- Four levers: streamlining workflows, aligning goals, reducing friction, and data-driven decision-making drive systemwide efficiency.
- Sustainable improvement requires a leadership mindset and ongoing evaluation, not one-time fixes.
What Is Healthcare Performance Improvement?
Healthcare performance improvement refers to the continuous efforts health systems make to enhance clinical outcomes, streamline workflows, reduce costs, and create more efficient, people-centered operations. It is not a one-time initiative, but a leadership-driven discipline grounded in data, strategy, and system-wide collaboration.
At its core, performance improvement asks a simple but powerful question: How can we deliver better care with fewer obstacles and more value?
Organizations focused on performance improvement typically aim to:
- Improve care delivery by minimizing variation and standardizing best practices
- Optimize workflows to reduce bottlenecks, delays, and rework
- Enhance patient outcomes through coordinated, high-quality care
- Control costs by eliminating waste and aligning resources more effectively
Across ambulatory care, tribal health, and behavioral health systems, performance improvement is essential for long-term sustainability. It enables leaders to respond to rising operational complexity, workforce shortages, and shifting reimbursement models with agility and foresight.
Importantly, performance improvement must be embedded into the organizational culture; not siloed to a single department or project team. When improvement becomes everyone’s responsibility, it drives smarter decisions, better patient experiences, and more resilient systems.
Many of the organizations we work with begin their improvement journey by focusing on a single domain, such as revenue cycle performance or clinical documentation. From there, small wins lead to broader transformation.
A behavioral health group we worked with began by making a small improvement in how they tracked key performance indicators starting with monitoring no-show rates for appointments. By implementing a simple reporting process and reviewing trends weekly, the team quickly identified gaps in reminder calls and patient engagement. This visibility not only helped reduce missed appointments but also highlighted other opportunities to measure and manage performance, such as clinician productivity and payer reimbursement trends. What began as a small data-tracking initiative evolved into a culture of data-driven decision-making, resulting in stronger operational oversight, better resource allocation, and a notable increase in revenue stability.
To create sustainable performance improvements, we often guide clients through a structured operational assessment. Our consultants at John Lynch & Associates examine what isn’t working, and why. This reveals hidden friction points and allows teams to address root causes, not just surface-level symptoms.
Ultimately, performance improvement isn't just about efficiency. It’s about building systems that support high-quality care, foster staff well-being, and deliver on your mission in an increasingly complex healthcare landscape.
For organizations seeking expert support in identifying inefficiencies, aligning teams, and implementing lasting change, our practice management consulting services offer a proven, people-first approach to driving performance at every level of the organization.
How to Improve Health System Performance
To improve health system performance, organizations must streamline workflows, align teams, reduce care delivery friction, and use data to guide decisions. These four levers enable leaders to build more efficient, resilient systems that improve care quality, reduce waste, and protect staff from burnout.
Streamlining Workflows to Reduce Waste
Every inefficient workflow hides time, money, and potential clinical risk. From intake to discharge, even small breakdowns (duplicative steps, redundant data entry, or delayed handoffs) add up to major losses in productivity and morale.
Streamlining workflows involves:
- Mapping end-to-end processes to uncover friction points
- Identifying non-value-added steps that can be automated, eliminated, or consolidated
- Standardizing best practices across care teams and locations
When done effectively, this doesn’t just increase speed, it improves consistency, reduces variation, and strengthens team trust.
One of our outpatient behavioral health clients began with a seemingly small improvement: reducing the time it took clinicians to complete progress notes after each session. By streamlining workflows and standardizing documentation templates, providers were able to finish charts more quickly, freeing up valuable time for patient care. What started as a time-saver for clinicians soon created ripple effects; documentation accuracy improved, claims were submitted faster, and denials dropped significantly. Within months, the clinic saw measurable gains in billing compliance and revenue capture, transforming what began as an operational efficiency project into a sustained increase in profitability and overall organizational performance.
Aligning Teams with Organizational Goals
Healthcare teams often work in silos; not because they want to, but because systems unintentionally disconnect their goals and communication pathways. Misalignment can lead to inconsistent performance, competing priorities, and lower staff engagement.
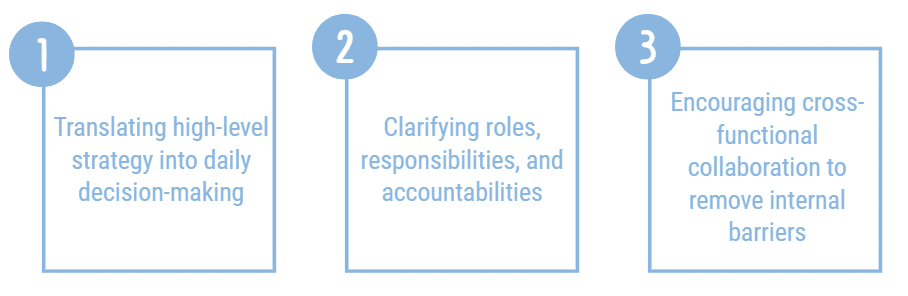
Improving performance requires clear alignment across clinical, operational, and administrative teams. This includes:
When everyone knows where the organization is headed, and how their role supports it, teams work with more focus, flexibility, and purpose.
Reducing Friction in Care Delivery
Even the best-intentioned clinical teams struggle when care delivery is bogged down by complexity. Friction shows up in multiple ways:
- Long wait times due to scheduling inefficiencies
- EHR workflows that require excessive clicks or duplicate documentation
- Poor care coordination between departments or providers
Removing friction in care delivery is both a performance and a patient experience imperative. It allows providers to spend more time on care (not navigation) and it leads to better clinical outcomes and higher patient satisfaction.
This is often where performance improvement efforts gain early traction, because small changes (like adjusting appointment templates or reworking intake forms) can deliver immediate relief.
Using Data to Drive Strategic Change
Data is the foundation of every effective performance improvement effort, but only when it’s used well. Many organizations collect plenty of data, but lack a unified approach to analysis, interpretation, and decision-making.
To drive change, we help clients:
- Establish relevant, role-specific KPIs for each department
- Create dashboards that provide real-time visibility into performance
- Use baseline and trend data to inform priorities and measure impact
Without reliable metrics, teams operate on assumptions. With data, they can make faster, smarter decisions that lead to sustained improvement. When organizations activate all four levers - streamlined workflows, team alignment, friction reduction, and data-driven change, they unlock scalable, repeatable improvements that benefit every stakeholder in the health system.
What Are Examples of Performance Improvement in Healthcare?
Healthcare organizations can achieve measurable gains by focusing on small, targeted improvements that build momentum over time. Below are common examples of performance improvement in healthcare settings:
- Reducing time to chart completion to accelerate billing and improve documentation quality
- Increasing clean claim rates by refining coding workflows and front-end accuracy
- Cutting patient wait times by redesigning scheduling templates and intake processes
- Improving clinical documentation to minimize audit risk and ensure compliance
- Streamlining staff onboarding to reduce ramp-up time and ensure role readiness
These outcomes are not the result of isolated initiatives; they’re often the product of coordinated, system-wide efforts grounded in operational insight and frontline feedback.
From Theory to Action
Many performance improvement projects begin with a single pain point. A clinic notices consistent delays in patient check-in. A behavioral health center faces recurring documentation backlogs. A tribal health facility struggles with claim rejections due to inconsistent coding.
In each case, the solution starts with an assessment of what’s happening behind the scenes.
- Are teams unclear on responsibilities?
- Is technology getting in the way?
- Are inefficient handoffs or redundant steps creating delays?
Even a small change, like redesigning an intake form, restructuring appointment templates, or standardizing documentation protocols, can yield significant impact. These actions reduce administrative burden, accelerate revenue capture, and give clinical teams more time to focus on patients.
What’s important is not just the tactic, but the approach. Organizations that commit to continuous improvement, rather than one-off fixes, create lasting systems that adapt to change, scale with growth, and protect against compliance risk.
For practical resources to support your own performance improvement efforts, the CDC Quality Improvement Toolkit offers helpful frameworks for tracking, measuring, and managing progress over time.

Why Time Management in Healthcare Drives Efficiency
Time is one of the most valuable and often most misused resources in healthcare. Poor time allocation leads to delayed care, higher costs, staff burnout, and ultimately, worse patient outcomes.
Healthcare performance improvement isn’t just about doing more with less. It’s about reclaiming time lost to inefficient processes, outdated systems, and misaligned roles. When leaders protect clinical and operational time through smart systems design, they unlock both quality and efficiency.
Administrative Time Is a Hidden Drain
For many providers and staff, the workday is filled with tasks that aren’t directly related to patient care. These administrative burdens often go unnoticed at the executive level, yet they have a cumulative, measurable impact.
Consider the following time drains:
- Complex EHR workflows that require excessive clicks and duplicative entry
- Manual handoffs that could be automated or simplified
- Inconsistent protocols that leave staff uncertain about next steps
- Multiple systems that don’t talk to each other, forcing workarounds
These issues not only eat into productivity, they also cause frustration, reduce focus, and increase the likelihood of error.
Improving time management begins by identifying where time is being lost and redesigning processes to make work easier, faster, and more predictable.
For one ambulatory care client, we helped reclaim significant staff time by redesigning their EHR scheduling and documentation processes. Previously, nurses and front-office staff were spending hours each week on manual appointment adjustments, duplicate data entry, and chasing incomplete provider notes. We streamlined the scheduling templates, optimized EHR workflows, and built in prompts to ensure complete documentation before chart closure. As a result, staff no longer needed to backtrack on missing information, providers reduced after-hours charting, and the front desk gained more time to focus on patient experience. This process redesign not only gave staff back valuable hours each week but also improved billing accuracy and patient throughput.
Improving Time Allocation Boosts Staff Retention
Time management is more than an operational issue. It’s also a workforce strategy.
When staff feel their time is valued, and when their workflows support rather than hinder them, they are more likely to stay engaged, satisfied, and committed to the organization.
We’ve seen firsthand how performance improvement initiatives that reduce administrative friction contribute to:
- Lower staff turnover
- Improved morale and job satisfaction
- Greater focus on clinical excellence
- Better patient-provider interactions
Especially in high-burnout environments like behavioral health or rural clinics, time-saving improvements are often the difference between staff staying or leaving.
Investing in better time allocation is not a short-term fix. It’s a long-term strategy for building a sustainable, high-performing workforce.
A Practical Framework for Healthcare Process Improvement
While every health system faces its own unique challenges, the path to meaningful performance improvement typically follows a predictable arc: assess the current state, align your teams and goals, and act with accountability and intention.
We use a three-phase framework: Assess → Align → Act, to help organizations move from insight to implementation in a way that’s sustainable, measurable, and centered on people.
This framework works across all care settings and organizational sizes, from tribal health centers and community clinics to large ambulatory systems and behavioral health networks.
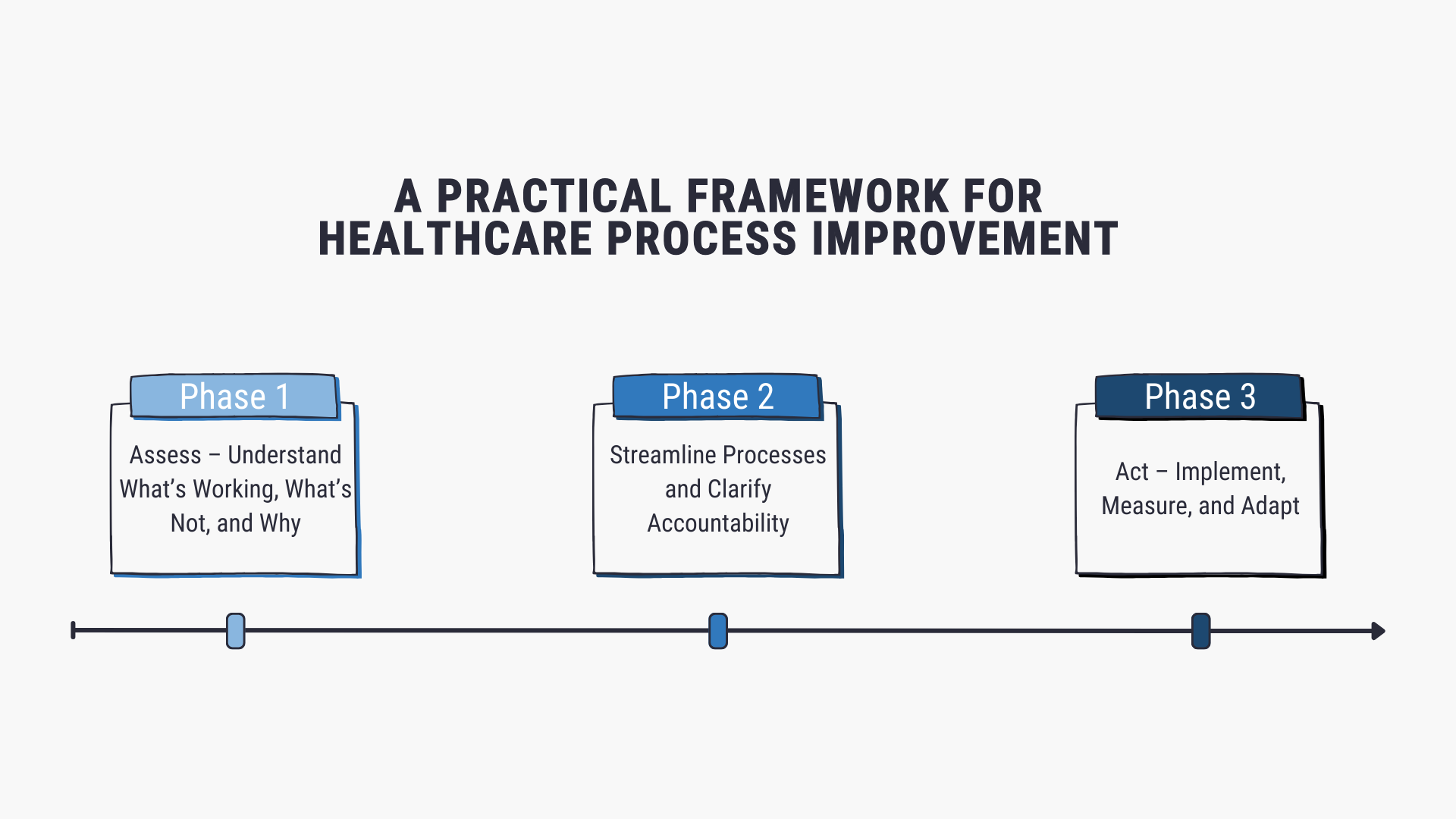
Phase 1: Assess – Understand What’s Working, What’s Not, and Why
Performance improvement starts with clarity. Before making changes, organizations need to understand the current state of operations—beyond surface-level metrics.
We guide teams through a comprehensive assessment using a combination of:
- Staff and stakeholder feedback (surveys, interviews, workshops)
- Workflow audits that trace clinical and administrative processes end to end
- Performance metrics (e.g., productivity, patient flow, claim denial rates)
This phase often reveals:
- Bottlenecks that delay care or increase costs
- Rework loops that waste time and frustrate staff
- Breakdowns in communication between departments or systems
- Missed benchmarks in areas like access, throughput, or compliance
And just as importantly, it helps surface cultural or organizational dynamics that may be holding teams back.
When assessing workflows, we also pay close attention to areas of compliance vulnerability, often a symptom of unclear processes or inconsistent documentation.
For more on compliance pitfalls and how they intersect with operational inefficiency, see Compliance Risk in Healthcare: 7 Emerging Threats to Watch
Phase 2: Align – Streamline Processes and Clarify Accountability
Once the root causes of underperformance are clear, the next step is aligning people, processes, and goals around a shared improvement strategy.
This phase includes:
- Clarifying roles and responsibilities across teams and departments
- Streamlining cross-functional processes to remove duplication and confusion
- Linking operational workflows to clinical, financial, and compliance outcomes
- Reinforcing shared accountability so that performance improvement isn’t siloed
Alignment creates a strong foundation for execution. It ensures that improvement is not just a leadership initiative, but a shared commitment across clinical, administrative, and operational teams.
In our experience, this phase is where many organizations see an immediate morale boost, because teams now have clarity, purpose, and support in doing their best work.
Phase 3: Act – Implement, Measure, and Adapt
In the final phase, we work with leadership teams to turn alignment into action by setting priorities, implementing change, and tracking results.
This includes:
- Prioritizing initiatives based on feasibility, impact, and urgency
- Assigning clear ownership for each improvement action
- Establishing KPIs and success metrics from the start
- Scheduling regular check-ins to evaluate progress and adjust course
Crucially, we help organizations resist the urge to launch too many initiatives at once. Focusing on a few high-impact changes creates momentum, demonstrates value, and builds confidence to scale.
This phase also reinforces that performance improvement is not a one-time project; it’s a cycle. As results come in, the organization re-enters the assessment phase with new data and new opportunities to refine and grow.
Whether your organization is looking to improve patient flow, reduce denials, or increase staff efficiency, this framework provides a structured, people-centered roadmap. It’s not about chasing quick wins. It’s about building the operational muscle to adapt, evolve, and lead.
Conclusion: Efficiency Is a Strategy, Not Just a Goal
Performance improvement is not just about getting faster. It’s about building healthcare systems that are smarter, stronger, and more responsive to the people they serve.
Inefficiencies don’t just waste time and money. They erode staff morale, compromise patient outcomes, and increase the risk of compliance violations. And in today’s healthcare environment, where every resource counts, those costs are too great to ignore.
The good news? Every organization has the potential to improve. It starts with asking the right questions:
- Where are we losing value?
- What’s slowing down our teams?
- Are our systems helping (or hurting) our mission?
By taking a structured, strategic approach to healthcare performance improvement, leaders can create real, measurable progress without overwhelming their staff or overextending their budgets. Whether you're aiming to reduce denials, streamline scheduling, or improve documentation workflows, the path to improvement is clear and achievable.
If you’re ready to uncover inefficiencies, align your team around shared goals, and build a smarter system for growth, our team is here to help. We bring operational expertise, clinical insight, and a people-first approach to every engagement.
Let’s build the kind of healthcare system your staff is proud to work in, and your patients trust to care for them.
Ready to Talk?
Further Reading
- CDC Performance Management and QI Hub - A collection of evidence-based tools, templates, and case studies to help health organizations adopt performance and quality improvement frameworks
Related Articles

The 5 Revenue Cycle Metrics Ambulatory Clinics Can’t Ignore During Peak Demand

Healthcare Performance Improvement: Proven Strategies for Operational Efficiency