Maximize Revenue Cycle Collections in Healthcare
Maximizing collection rates is a critical component of healthcare revenue cycle management, ensuring that healthcare providers can maintain financial stability while continuing to offer high-quality patient care.
Let’s dive into the revenue cycle process and discuss effective strategies essential for optimizing collections, reducing errors, and improving the overall efficiency of the billing process.
Article Highlights
-
Proactive patient communication improves upfront collections and reduces billing delays.
-
Accurate insurance verification and eligibility checks prevent costly claim denials and rework.
-
Streamlined billing and coding practices increase first-pass claim acceptance rates and speed up reimbursements.
-
Staff training and accountability programs strengthen revenue cycle performance across the organization.
-
Regular performance monitoring and KPIs ensure continuous improvement and long-term financial success.
Understanding Revenue Cycle in Healthcare
Defining the Healthcare Revenue Cycle
At its core, the healthcare revenue cycle is the holistic process through which healthcare providers receive payment for the services they offer. It includes various critical stages such as patient registration, insurance verification, service documentation, coding, and billing, claim processing, payment collection, and the management of denied claims.
Each step is interconnected, and any inefficiencies or errors can lead to delays, denials, and ultimately, a decrease in the collection rate.
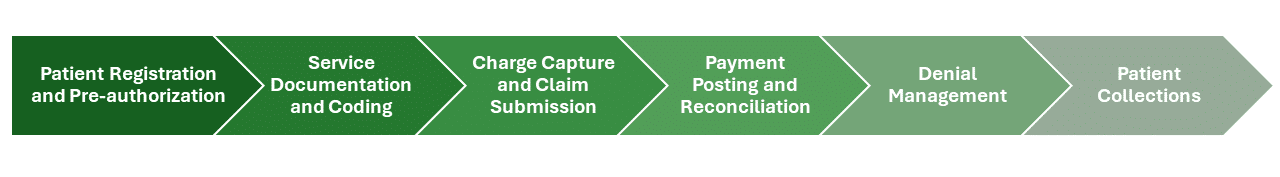
Steps Involved in the Revenue Cycle
- Patient Registration and Pre-authorization: This initial step involves gathering patient demographic and insurance information. Accurate data collection at this stage is crucial to ensure eligibility and secure pre-authorizations if necessary.
- Service Documentation and Coding: After the patient receives care, the services provided are documented and translated into standardized codes. These codes are essential for billing and determine the reimbursement amount from insurers.
- Charge Capture and Claim Submission: Charges for the services are captured, compiled, and submitted to the insurance company in the form of a claim. This step requires meticulous attention to detail to avoid errors that could lead to claim denials.
- Payment Posting and Reconciliation: Payments received from insurers and patients are posted to their respective accounts. This stage involves reconciling the amounts paid against the amounts billed to ensure accuracy.
- Denial Management: Denied claims are reviewed, corrected, and resubmitted. Effective denial management strategies are vital for recovering revenue that would otherwise be lost.
- Patient Collections: Finally, any remaining balances after insurance payments are collected directly from the patients. This step involves clear communication and flexible payment options to facilitate patient payments.
Impact of Collections on Financial Performance
The efficiency of the revenue cycle directly impacts a healthcare provider’s financial performance. High collection rates signify a healthy revenue cycle, enabling providers to cover operational costs, invest in new technologies, and expand patient care services. Conversely, poor collection practices can lead to financial strain, affecting a provider’s ability to deliver quality care.
To navigate the complexities of the revenue cycle successfully, healthcare providers must adopt a proactive and patient-centered approach. This involves implementing robust processes for each step of the cycle, leveraging technology to streamline operations, and maintaining transparent communication with patients about their financial responsibilities.
By doing so, healthcare providers can enhance their collection rates, ensuring financial stability and the continued provision of high-quality healthcare services.

Common Challenges Affecting Collection Rates
Common Collection Process Challenges
- Denied Claims: One of the most significant challenges in the revenue cycle is the high rate of claim denials by insurance companies. Denials can occur for several reasons, including coding errors, lack of pre-authorization, and incorrect patient information. Each denied claim requires additional resources to correct and resubmit, delaying payment and affecting cash flow.
- Coding Errors: Accurate medical coding is crucial for the billing process. Coding errors can lead to claim denials or underpayment for services rendered. Keeping up with frequent changes in coding standards and regulations requires continuous education and training for coding staff.
- Inefficient Billing Processes: Manual billing processes and outdated technology can lead to inefficiencies, such as slow claim submission, errors in billing statements, and difficulties in tracking the status of claims and payments.
- Patient Payment Collection Issues: Increasing patient responsibility due to high-deductible health plans and other factors has made patient collections more challenging. Patients may be unable or unwilling to pay their portion of the bill, leading to outstanding balances and increased collection efforts.
- Lack of Transparency: Patients often find healthcare billing confusing and lack understanding of their financial responsibility. This lack of transparency can lead to dissatisfaction, disputes, and delays in payment.
Strategies for Maximizing Collection Rates
Accurate Patient Registration and Data Collection
Ensuring accurate collection of patient information, including insurance details at the point of registration. This step is critical for verifying eligibility and securing authorization for services.
Outcome: Minimizes claim denials due to incorrect patient information or insurance details, streamlining the billing process and enhancing collection rates.
Effective Claims Management
Implementing a robust claim management process that includes regular audits, timely submission, and systematic follow-up on unpaid claims. It also involves analyzing denial patterns to prevent future occurrences.
Outcome: Reduces the number of denied and unpaid claims, improving the overall efficiency of the billing process and ensuring more consistent revenue flow.
Utilize Predictive Analytics
Leveraging predictive analytics to analyze patient data and historical billing information to forecast potential payment issues or identify patients who may require financial assistance or tailored payment plans.
Outcome: Allows for proactive management of collections, reducing the number of accounts that become delinquent and enabling targeted interventions to improve collection efforts.
Streamline Patient Payment Processes
Simplifying the payment process for patients by offering multiple payment options, including online portals, mobile payments, and flexible payment plans. Ensuring billing statements are clear, concise, and easy to understand.
Outcome: Increases the likelihood of timely patient payments by accommodating diverse patient preferences and financial situations, thereby improving collection rates.
Staff Training and Education
Providing ongoing training and education for staff on the latest billing practices, coding updates, and technology tools. This includes training on patient communication skills to handle financial discussions sensitively and effectively.
Outcome: Ensures billing and coding accuracy, enhances operational efficiency, and improves patient interactions related to billing inquiries and payment negotiations.
Patient Education and Communication
A crucial aspect of addressing collection challenges is improving patient education and communication regarding financial responsibilities. Providing patients with estimates before service and offering flexible payment plans can also enhance patient satisfaction and willingness to pay.
Outcome: Clear, transparent communication about the cost of services, insurance coverage, and payment options can help mitigate payment delays and disputes.
By adopting these strategies, healthcare providers can address the multifaceted challenges of revenue cycle management. Implementing advanced technology, optimizing processes, and focusing on patient engagement not only improves collection rates but also contributes to the overall financial health of healthcare organizations.

The Role of Technology in Maximizing Collections
The dynamic landscape of healthcare revenue cycle management continues to evolve, with technology playing an increasingly pivotal role in maximizing collection rates. The adoption of advanced technology solutions not only streamlines the billing and collection processes but also enhances accuracy, reduces errors, and improves patient satisfaction.
Let’s explore the transformative impact of technology on healthcare revenue management and how it paves the way for more efficient and effective collection strategies.
Electronic Health Records (EHR) Integration
Integrating billing systems with your EHR ensures that clinical and billing processes are seamlessly connected. This integration facilitates the automatic transfer of patient information and service details to the billing system, reducing manual data entry and the associated errors.
Impact: EHR integration streamlines the billing process, enhances data accuracy, and speeds up claim submission. It also improves the tracking of patient care activities, ensuring that all billable services are accurately captured and billed.
Automated Claims Submission and Processing
Automated claim submission tools allow healthcare providers to submit claims electronically, directly to payers. These systems often include features for checking claims against payer rules before submission, identifying potential errors or issues that could lead to denials.
Impact: Automation reduces the time and effort required to submit claims, decreases the rate of claim denials due to errors, and accelerates the reimbursement process. It also frees up staff to focus on more complex tasks and patient care.
Predictive Analytics for Revenue Optimization
Predictive analytics uses historical data and machine learning algorithms to forecast future billing outcomes, identify potential issues before they arise, and optimize the revenue cycle. This can include predicting patient payment behavior, identifying high-risk accounts, and optimizing pricing strategies.
Impact: By leveraging predictive analytics, healthcare providers can proactively address potential revenue cycle issues, tailor their collection strategies to individual patient needs, and make informed decisions about financial policies and procedures.
Patient Engagement Platforms
Patient engagement platforms – also known as patient portals enhance communication between healthcare providers and patients regarding financial obligations. These platforms may offer features such as online bill pay, payment plan management, and electronic statements, making it easier for patients to understand and fulfill their payment responsibilities.
Impact: Improved patient engagement leads to higher patient satisfaction, increased transparency about costs, and a higher likelihood of on-time payments. These platforms also reduce the administrative burden on staff by automating many patient communication tasks.
Denial Management Software
Denial management software helps healthcare providers identify, track, and manage denied claims. These systems can analyze patterns in denials to pinpoint underlying issues, facilitating targeted improvements in the billing process.
Impact: Effective denial management ensures quicker resolution of denied claims, improving cash flow, and reducing the revenue lost to unaddressed or unresolved denials. It also helps in refining billing practices to prevent future denials.
Integrating technology into healthcare revenue cycle management offers many benefits, from operational efficiencies and reduced errors to improved patient engagement and satisfaction.
As healthcare providers navigate the complexities of the modern billing landscape, embracing these technological solutions is essential for maximizing collection rates and ensuring financial stability.
The future of healthcare revenue cycle management lies in the strategic use of technology to enhance every aspect of the billing and collection process, driving better outcomes for providers and patients alike.

Future Trends in Healthcare Revenue Cycle Management
The healthcare revenue cycle is undergoing a significant transformation, driven by technological advancements, regulatory changes, and evolving patient expectations. As we look to the future, several key trends are poised to shape the landscape of healthcare revenue cycle management.
These trends underscore the need for adaptability, innovation, and patient-centric approaches in optimizing financial performance and enhancing patient care.
Emphasis on Patient-Centric Billing
There’s a growing shift towards more transparent, understandable, and patient-friendly billing processes. This trend is driven by the increasing role of patients as active consumers in their healthcare decisions, demanding clarity and convenience in billing and payments.
Implications: Healthcare providers will need to focus on improving the patient’s financial experience through clear communication, straightforward billing statements, and flexible payment options. Success in this area will not only improve collections but also patient satisfaction and loyalty.
Integration of Artificial Intelligence (AI) and Machine Learning (ML)
Artificial intelligence and machine learning are becoming integral to automating complex processes, analyzing vast amounts of data for insights, and personalizing patient interactions. These technologies can streamline billing and coding, predict payment issues, and optimize revenue cycle strategies.
Implications: The adoption of AI and machine learning will enable healthcare providers to identify and address inefficiencies in the revenue cycle, tailor financial interactions to individual patient needs, and proactively manage risks related to billing and collections.
Increased Use of Telehealth
The rapid adoption of telehealth has introduced new challenges and opportunities in billing and reimbursement. As telehealth becomes a permanent fixture in healthcare delivery, providers must navigate the intricacies of billing for virtual visits and ensure compliance with payer policies.
Implications: Healthcare organizations will need to adapt their billing practices to accommodate telehealth services, including staying updated on coding changes and payer guidelines. This will require ongoing education and training for billing staff and investment in technology that supports telehealth billing.
Focus on Value-Based Care
The shift towards value-based care models emphasizes outcomes and patient satisfaction over the volume of services provided. This trend impacts the revenue cycle by aligning financial incentives with the quality of care, requiring providers to demonstrate the value of their services.
Implications: Success in a value-based care environment will depend on the ability to efficiently collect and analyze data on patient outcomes and satisfaction. Providers will need to invest in technology and processes that support outcome-based billing and demonstrate the quality of care to payers and patients.
Regulatory Compliance and Transparency
Regulatory requirements are evolving to promote greater transparency in healthcare pricing and billing practices. Compliance with these regulations not only affects legal and financial risk but also patient trust and satisfaction.
Implications: Healthcare providers must ensure that their billing practices comply with current regulations and are prepared to adapt to future changes. This includes transparent pricing, accurate and understandable billing statements, and clear communication about financial policies.
As these trends continue to evolve, healthcare providers must remain agile, leveraging technology and data to navigate the changing landscape. By focusing on efficiency, transparency, and patient engagement, providers can enhance their revenue cycle management processes, improve collection rates, and deliver better care to their patients.

The Role of Revenue Cycle Consultants
Our revenue cycle consultants offer specialized knowledge and experience that can help your healthcare organization navigate the complexities of the revenue cycle. Our consultants bring a fresh perspective, identifying inefficiencies and opportunities for improvement that may not be apparent to internal teams. With their expertise, our consultants can:
- Implement Best Practices: They can introduce proven strategies and best practices for every aspect of the revenue cycle, from patient registration and billing to collections and denials management.
- Leverage Technology: Consultants can guide the selection and implementation of the latest technology solutions, ensuring that healthcare providers benefit from the efficiencies and insights that these tools offer.
- Enhance Patient Engagement: By focusing on the patient financial experience, consultants can help develop strategies that improve transparency, communication, and satisfaction, directly impacting collection rates.
- Navigate Regulatory Changes: With their up-to-date knowledge of regulatory requirements, consultants can ensure that healthcare providers remain compliant, avoiding penalties and fostering trust.
- Optimize Financial Performance: Ultimately, the goal of revenue cycle consultants is to enhance the financial health of healthcare organizations, enabling them to focus on their core mission of providing excellent patient care.
As healthcare continues to evolve, the expertise and guidance of revenue cycle consultants will be more critical than ever. They can provide the strategic insight and operational support necessary to navigate the challenges ahead, ensuring that healthcare providers can adapt, thrive, and continue to deliver the highest quality of care.
Conclusion
The landscape of healthcare revenue cycle management is continuously evolving, influenced by emerging trends such as patient-centric billing, the integration of AI and machine learning, the expansion of telehealth, the shift towards value-based care, and the imperative for regulatory compliance and transparency.
In this dynamic environment, healthcare providers face the daunting task of adapting to change while maintaining the highest standards of patient care. It’s a balancing act that requires not only operational efficiency and financial acumen but also a deep understanding of the patient experience. John Lynch & Associates is here to help - contact us today to get started.
Ready to talk?

3 Strategies to Improve Behavioral Health Financial Stability

Is Your Ambulatory Practice Leaving Money on the Table? Here’s How to Fix That



