Every minute lost to inefficient EHR workflows in behavioral health isn’t just a frustration it’s a direct hit to financial stability, clinician well-being, and patient care.
When providers spend extra time clicking through screens, searching for patient history, or correcting documentation errors, they lose billable hours, delay treatment, and increase burnout. Multiply this across an organization, and the costs become staggering longer wait times, higher patient dropout rates, and mounting administrative expenses.
At John Lynch & Associates, we’ve seen firsthand how inefficient EHR workflows create these challenges. As a consulting firm specializing in behavioral health IT strategy and workflow optimization, we help organizations identify bottlenecks, streamline processes, and implement tailored solutions that improve both financial and clinical outcomes.
Even small changes such as reducing redundant data entry or optimizing templates can save hundreds of hours per year, leading to higher revenue, reduced administrative burden, and greater clinician satisfaction.
In this article we’ll break down the hidden costs of inefficient EHR workflows, illustrate their impact with real-world examples, and explore actionable solutions to improve EHR usability, increase efficiency, and enhance care quality.
The Cost of Inefficient EHR Workflows
Understanding the Scope of the Problem
Behavioral health providers face unique challenges that make EHR workflow inefficiencies particularly harmful. Unlike many other healthcare fields, behavioral health requires extensive documentation, covering not only clinical notes but also detailed progress reports, treatment plans, and compliance documentation. Additionally, behavioral health often involves longitudinal care, meaning patient records must be comprehensive, accurate, and easily accessible across multiple encounters and providers.
However, many EHR systems were not originally designed for behavioral health needs, leaving providers with cumbersome documentation processes, poor system interoperability, and redundant data entry. These inefficiencies slow down patient intake, disrupt continuity of care, and create administrative bottlenecks that take time away from actual patient treatment.
Without intuitive, integrated workflows, clinicians are forced to navigate fragmented data systems, delayed care coordination, and disjointed communication between providers. When vital patient history is inaccessible or scattered across multiple platforms, it leads to documentation errors, slower response times, and gaps in treatment planning. These challenges, highlighted in federal reports on behavioral health IT adoption, reveal how poor EHR usability increases administrative burdens and disrupts the delivery of timely, high-quality care.
Financial Impact
When EHR workflows are inefficient, the financial losses add up quickly. Here’s how:
- Missed Billing Opportunities: Inaccurate or incomplete documentation can lead to claim denials, delaying or forfeiting revenue.
- Extended Claims Processing Times: If workflows slow down billing submission or require frequent manual corrections, reimbursement cycles become longer.
- Increased Administrative Costs: When clinicians spend excessive time on documentation, organizations must often hire additional administrative support, raising operational expenses.
For example, a mid-sized behavioral health clinic with ten clinicians spending just 20 extra minutes per day on documentation inefficiencies could see a loss of over 16 billable hours per week. If each billable hour is valued at $150, that’s nearly $2,500 per week in lost revenue or more than $120,000 annually. And that’s just one example.
Clinical Impact
Beyond financial loss, workflow inefficiencies directly impact patient care by creating:
- Delays in Treatment: When documentation takes too long, providers have less time for patient interactions and treatment planning.
- Fragmented Data Sharing: When systems don’t communicate properly, critical patient information can be lost or inaccessible, leading to uninformed clinical decisions.
- Higher Patient Dropout Rates: Long intake processes, scheduling inefficiencies, and lack of follow-up reduce patient engagement, increasing dropout rates.
For example, if a patient struggling with depression waits weeks for an appointment due to scheduling inefficiencies, they may disengage from care altogether. The same applies to patients with substance use disorders, where immediate intervention can be the difference between relapse and recovery.
Emotional Toll on Staff and Patients
Clinician burnout in behavioral health is at an all-time high, and inefficient EHR workflows are a major contributor. When providers spend more time fighting technology than treating patients, frustration rises. Studies show that cumbersome EHR systems increase emotional exhaustion, reduce job satisfaction, and contribute to high turnover rates.
From the patient’s perspective, inefficient workflows lead to long wait times, repeated intake questions, and difficulty accessing care, all of which erode trust. Behavioral health care relies heavily on strong patient-provider relationships, and workflow inefficiencies put those relationships at risk.

Real-World Examples of Workflow Inefficiencies
The Domino Effect of Inefficiency
Inefficient EHR workflows don’t just slow down individual providers they create a chain reaction that affects the entire organization. Consider a behavioral health clinic struggling with manual data entry, fragmented communication, and scheduling backlogs.
A therapist spends extra time searching for notes or re-entering information, leading to longer patient wait times and fewer available appointment slots. As a result, patients disengage from care, while the clinic loses revenue from missed or canceled appointments.
For many behavioral health organizations, inefficiency starts at intake. Lengthy, redundant forms frustrate new patients, increasing the likelihood of no-shows before treatment even begins. A study by the National Council for Mental Wellbeing found that 46% of behavioral health patients abandon care before their third session, often due to friction in scheduling, intake, and communication. An inefficient EHR workflow that fails to support automated appointment reminders, streamlined intake forms, or real-time clinician scheduling contributes to this problem.
The right EHR optimization strategy can turn this around. Our guide, Choosing the Best EHR for Your Behavioral Health Clinic, offers guidance on selecting systems designed to reduce these inefficiencies, improving patient retention and clinician efficiency.
Impact on Organizational Stability
Beyond lost revenue and patient frustration, workflow inefficiencies threaten long-term organizational stability. High administrative burden and poor EHR usability contribute to clinician burnout, which is one of the leading causes of staff turnover in behavioral health.
A 2022 survey found that 60% of behavioral health professionals reported symptoms of burnout, with EHR-related frustration ranking among their top concerns. When staff leave due to poorly optimized systems, organizations face the high cost of recruitment, training, and lost productivity.
At John Lynch & Associates, we’ve helped behavioral health organizations navigate these challenges by identifying workflow gaps and implementing tailored EHR solutions. A mid-sized behavioral health clinic in Arizona was struggling with inconsistent billing processes, leading to revenue delays and compliance risks with AHCCCS requirements.
We conducted a thorough assessment of their Revenue Cycle Management (RCM) workflow and identified inefficiencies in claims submission, denials management, and credentialing.
By implementing standardized billing protocols, automating key RCM processes, and providing staff training on AHCCCS guidelines, the clinic saw a 25% reduction in claim denials and a 30% improvement in cash flow within six months. Additionally, our compliance team helped the organization establish internal auditing procedures, ensuring long-term adherence to regulatory requirements.
As a result, the clinic was able to expand services, reduce administrative burdens, and focus on patient care, knowing their financial and operational foundations were stable and optimized.
The ROI of EHR Workflow Optimization
Tools and Metrics for Measuring ROI
For behavioral health organizations, optimizing EHR workflows isn’t just about improving efficiency it’s a financial necessity. Measuring the return on investment (ROI) of workflow optimization requires tracking key performance indicators (KPIs) that reflect both operational and clinical efficiency. Some of the most critical EHR workflow metrics include:
- Time spent on documentation per session: Reducing the time clinicians spend on manual data entry allows for more patient interactions.
- Billing error rates and reimbursement cycle times: Streamlined workflows ensure accurate, timely billing and fewer claim denials.
- No-show and patient dropout rates: More efficient scheduling and intake processes lead to better patient retention.
- Clinician satisfaction and retention metrics: Less time spent struggling with inefficient systems results in lower burnout rates and higher staff retention.
Healthcare organizations that optimize EHR workflows experience significant cost savings by reducing administrative burden and improving overall revenue cycle management (source). By implementing data-driven workflow improvements, organizations can quantify the impact of their changes and continuously refine their systems for long-term efficiency.
Tangible Benefits of Optimization
When behavioral health organizations invest in EHR workflow optimization, the benefits are both immediate and long-term:
- 30-50% reduction in documentation time: Providers spend more time with patients instead of navigating complex EHR interfaces.
- Faster claim approvals and increased revenue: Optimized workflows reduce coding errors and streamline the claims process.
- Lower clinician burnout rates: Efficient, user-friendly EHR systems lead to higher job satisfaction and lower staff turnover.
- Improved patient engagement and retention: Shorter intake times and more efficient scheduling reduce patient frustration and increase adherence to treatment plans.
Emerging AI-driven tools are also making EHR workflow optimization even more impactful. By leveraging automation for data entry, predictive scheduling, and real-time clinical decision support, organizations can significantly enhance efficiency while maintaining high-quality care.
Strategies and Solutions for Behavioral Health Workflow Optimization
Practical Steps for Improvement
Optimizing EHR workflows in behavioral health isn’t just about reducing frustration it’s about creating a system that supports clinicians, enhances efficiency, and ultimately improves patient care. Organizations that take a proactive, structured approach to workflow optimization see measurable improvements in documentation time, billing accuracy, and patient retention. Here are some of the most effective strategies:
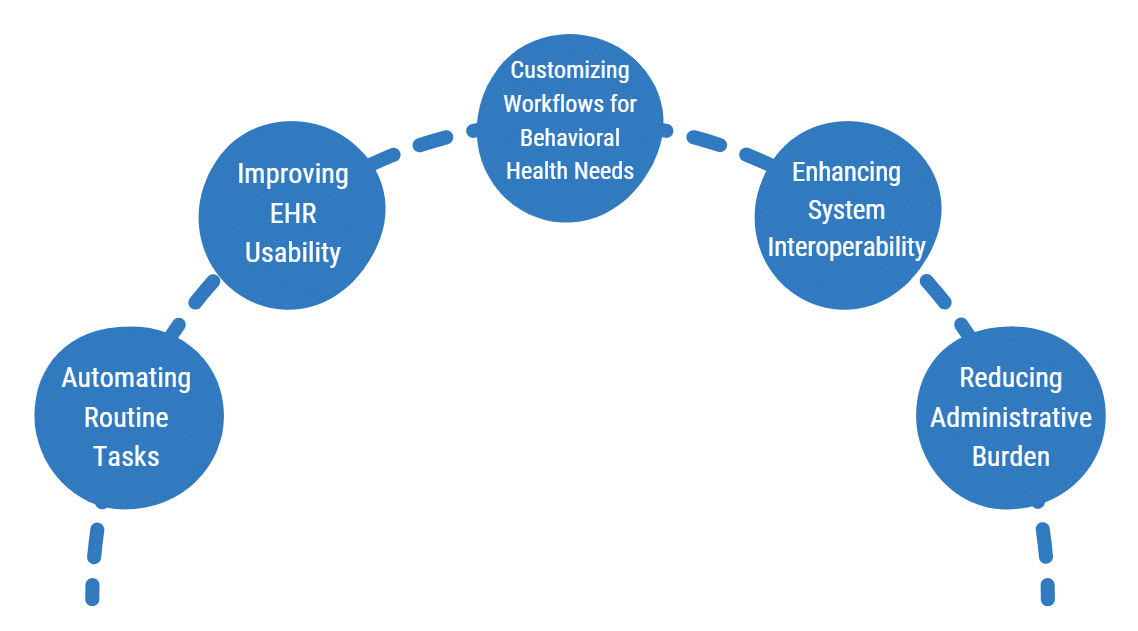
- Automating Routine Tasks: Reducing manual data entry and leveraging EHR automation for appointment scheduling, documentation, and claims processing saves valuable time and reduces errors.
- Improving EHR Usability: Training staff on workflow shortcuts, template customization, and voice-to-text documentation can significantly decrease time spent navigating the system.
- Customizing Workflows for Behavioral Health Needs: Unlike general medical practices, behavioral health requires detailed progress notes, treatment plans, and compliance tracking. Configuring EHR workflows to align with these needs eliminates unnecessary steps and streamlines processes.
- Enhancing System Interoperability: Ensuring seamless integration with labs, primary care providers, and other health systems improves data sharing and care coordination, reducing duplicate documentation.
- Reducing Administrative Burden: Identifying and eliminating redundant tasks helps clinicians focus on patient care rather than excessive paperwork.
Targeted EHR workflow solutions have been shown to improve efficiency, patient access, and clinician satisfaction, making these changes an essential investment.
Partnering for Success
While many behavioral health organizations recognize the need for EHR workflow optimization, the challenge lies in implementation. Without expert guidance, it’s easy to overlook key inefficiencies or struggle with system configurations that don’t fully align with an organization’s needs.
At John Lynch & Associates, we work closely with behavioral health leaders to evaluate current workflows, identify inefficiencies, and implement tailored solutions that improve both clinical and financial performance. From EHR system selection to customized workflow redesign, our approach ensures that behavioral health organizations maximize efficiency while maintaining compliance and quality of care.
A community-based behavioral health clinic in Arizona faced operational inefficiencies that impacted both revenue and patient care. Their biggest challenges included delayed claims processing, inefficient intake procedures, and inconsistent documentation practices, leading to cash flow issues and compliance risks with AHCCCS.
Our Approach
John Lynch & Associates conducted a comprehensive workflow analysis and identified key inefficiencies in their Revenue Cycle Management (RCM), patient intake, and documentation workflows. Our team implemented:
- Automated billing and claims tracking to reduce denials and accelerate reimbursements
- Standardized intake and documentation protocols to improve efficiency and reduce errors
- Staff training on compliance best practices to minimize audit risks
Measurable Outcomes
- 40% reduction in claim denials due to improved coding and documentation
- 30% increase in monthly revenue by optimizing billing workflows and reducing delays
- 25% faster intake process, allowing clinicians to focus more on patient care
- 100% compliance with AHCCCS billing and documentation standards
The result? The clinic saw a dramatic improvement in financial stability, reduced administrative burden, and improved patient service delivery. By streamlining their workflows, they were able to hire additional staff, expand services, and focus on delivering high-quality behavioral healthcare.
For organizations looking to create a long-term strategy for workflow optimization, having a clear roadmap is key. A well-planned strategy ensures sustainable improvements and ongoing success.
Conclusion
Inefficient EHR workflows are more than just an operational nuisance, they pose a serious threat to financial sustainability, clinician well-being, and patient outcomes. From lost revenue and delayed care to clinician burnout and high patient dropout rates, the hidden costs of inefficiency can quietly undermine a behavioral health organization’s success.
The good news? These inefficiencies are fixable. By implementing targeted EHR workflow solutions, automating repetitive tasks, and improving system usability, organizations can increase efficiency, reduce administrative burden, and enhance patient care. The return on investment is clear: optimized workflows lead to higher revenue, reduced staff turnover, and improved patient retention.
At John Lynch & Associates, we specialize in helping behavioral health organizations streamline their EHR workflows, eliminate inefficiencies, and create sustainable solutions tailored to their unique needs. Whether it’s customizing documentation templates, improving interoperability, or designing a long-term optimization strategy, we work alongside leadership teams to ensure meaningful, lasting improvements.
Behavioral health leaders who prioritize EHR workflow optimization today will be the ones best positioned for financial stability, improved care quality, and long-term success. The time to act is now.
Ready to Talk?